Moffitt Develops COVID-19 Testing for Patients
As cases of COVID-19 in the Tampa Bay area increased, so did the need for a fast, accurate test for the virus.
Moffitt Cancer Center’s Molecular Diagnostic Laboratory usually performs gene mutation tests for tumors, not tests for things like microorganisms and viruses.
But researchers used the technology and resources they already had to get a COVID-19 test up and running for Moffitt patients.

Dr. Dahui Qin, Medical Director of the Morsani Molecular Diagnostics Laboratory
“The entire cancer center was mobilized for this,” said Dr. Dahui Qin, medical director of the Morsani Molecular Diagnostics Laboratory.
The pathology department joined forces with the Microbiology Lab, which has expertise in handling viral specimens, and the state-of-the-art technology of the Molecular Diagnostic Lab, to bring in the COVID-19 test.
“Because the coronavirus that causes COVID-19 is new and the viral test is new to our lab, we reached out to internal and external experts for advice on how to do this test safely,” Qin said.
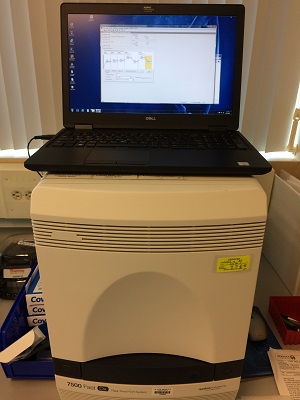
Machine used to run COVID-19 tests at Moffitt
The labs identified and obtained the proper COVID-19 test kit and positive samples and worked quickly to validate the test, which took about five days.
The test is called a polymerase chain reaction, or PCR. If clinicians suspect a patient has COVID-19, they can take a sample from the patient’s nasopharynx—the upper part of the throat behind the nose—using a swab through the nose. That swab is sent to the Microbiology Lab, where technologists extract ribonucleic acid, or RNA, from the sample and then test for the virus.
It takes about two hours to run the real-time PCR part of the test, and depending on when the test is run, patients can get results the same day or the next day.

Dr. John Greene, Chair, Infectious Disease Department
“Testing has ramped up dramatically so that we can actually run a larger number of tests and get results back the same day,” said Dr. John Greene, chair of Moffitt’s Infectious Disease Department. “A month ago, we had to send the test to an outside lab and it would take up to 14 days to get those tests back.”
Moffitt’s lab also runs control tests alongside the COVID-19 test to make sure the test is running correctly and to help identify any false positive or false negative results.
The PCR test is more accurate than the much-publicized rapid five-minute tests, which received emergency-use authorization from the U.S. Food and Drug Administration at the end of March. The rapid tests look for a specific antigen and carry a higher risk of false negative results.
“If the result of an antigen test is positive, you can stop there and be treated,” said Greene. “But if it’s negative, it’s not really a guarantee that you don’t have the virus. You would need to have a more sophisticated test like the PCR.”

No matter the testing method, someone with COVID-19 can still test negative if the concentration of the virus inside the body isn’t high enough at the time of the test. If symptoms persist and an individual is retested after the virus has multiplied over several days, the test could turn positive.
Researchers around the country also are working hard on an antibody test. Instead of detecting the virus inside the body like the PCR and antigen tests, an antibody test can determine if an individual has had the virus and has developed immunity against getting it again.
Once available, an antibody test can be used on healthcare workers in Florida to determine who is protected from the virus and can take care of patients without concerns about catching it.



