Triple Negative Breast Cancer Treatment Information
Triple negative breast cancer comprises approximately 10-15% of all breast cancer cases and differentiates itself with several key characteristics. Most notably, when triple negative cell samples are analyzed in a lab, the pathology results reveal an absence of three hormone receptors—estrogen, progesterone and the HER2 protein—which usually exist in healthy breast cells. As such, hormone therapy and medicines that target HER2 protein receptors are not effective against this type of cancer. Triple negative breast cancer is also more aggressive and has a higher grade than other breast cancers. (Cancer cells can be graded on a scale of 1 to 3, depending on how closely they resemble healthy breast cells; triple negative breast cancer is usually a grade 3 cancer.)
Common symptoms of triple negative breast cancer
The symptoms of triple negative breast cancer are similar to those of other forms of breast cancer. Individuals may experience:
- Breast lumps or masses (felt on or within the breast)
- Breast asymmetry
- An “orange peel” texture to the breast skin
- Redness or swelling of the breast
- Flaking or peeling nipples
- Nipple discharge (not associated with breast milk)
- Breast irritation, itchiness, warmth or pain
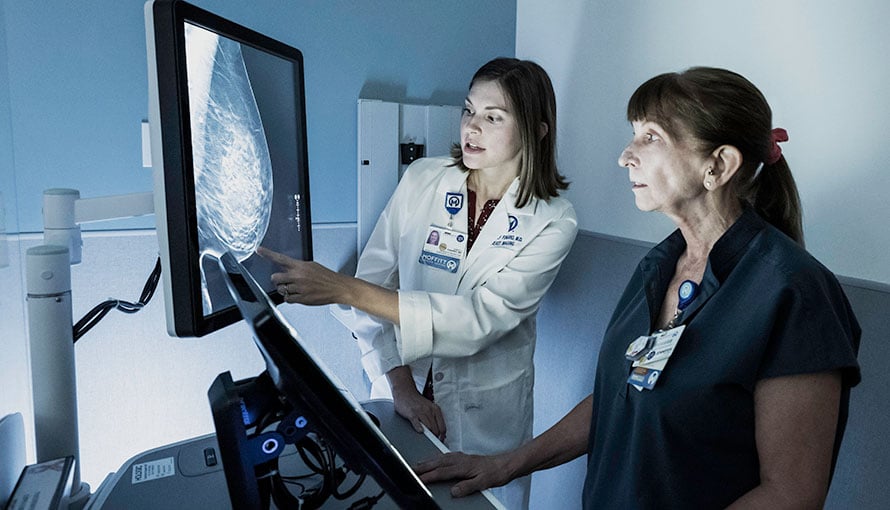
How triple negative breast cancer is diagnosed
Breast cancer is often diagnosed using imaging tests and a biopsy. Some of the most common diagnostic tools for breast cancer include:
- Mammograms – Digital mammography and full-breast tomosynthesis may be used to take X-rays of the breast from several angles.
- Breast ultrasounds – During a breast ultrasound, penetrating sound waves make computerized pictures of the inside of the breast. Ultrasounds provide a much clearer image of breast tissue than mammograms and can define whether a mass is solid or filled with fluid.
- Magnetic resonance imaging (MRI) – An MRI is not always necessary to diagnose breast cancer, especially if the breast ultrasound was conclusive. But it can be a helpful screening tool for those with a higher-than-average risk for breast cancer.
- Biopsies – Fine-needle aspirations, core-needle biopsies, stereotactic biopsies and surgical biopsies can be used to confirm a breast cancer diagnosis. During this procedure, tissue or fluid is removed from the breast and then analyzed under a microscope.
If breast cancer is the confirmed diagnosis after imaging tests and a biopsy have been done, the breast cancer cells will be sent to a lab to be analyzed. If the cells do not have progesterone and estrogen hormone receptors or an excess amount of the HER2 protein, the resulting diagnosis is triple negative breast cancer.
Triple negative breast cancer treatment
When formulating a treatment plan, oncologists will take the triple negative diagnosis into significant consideration. The reason is that traditional hormone-based therapies like tamoxifen and Herceptin, which are often helpful for treating hormone-receptive breast cancers, do not affect triple negative breast cancer. Typically, triple negative breast cancer is treated with one or more of the following methods:
- Surgery – A lumpectomy or mastectomy procedure can be used to remove as much of a tumor as possible.
- Radiation therapy – Targeted, high-energy rays are used to destroy breast cancer cells.
- Chemotherapy – Drugs are administered to destroy rapidly dividing cancer cells.
- Neoadjuvant therapy – Chemotherapy or radiation therapy is administered before or after surgery.
Some patients wonder whether triple negative breast cancer should be treated more aggressively than other types of breast cancer. This is not necessarily the case. In fact, some researchers believe that triple negative breast cancer responds more favorably to chemotherapy than hormone-receptive cancers.
Risk factors for triple negative breast cancer
A risk factor is a characteristic that increases an individual’s chance of getting a certain condition. For example, cigarette smoking is a risk factor for lung cancer. While anyone can receive a diagnosis of triple negative breast cancer, it is more likely to affect the following individuals:
- Those who are younger than age 40
- Those who have the BRCA1 mutation
- Those of African-American or Hispanic descent
Having one or more of these risk factors does not mean developing triple negative breast cancer is for certain, just as not having any of these risk factors doesn’t prevent an individual from being diagnosed with this condition.
Triple negative breast cancer recurrence
Triple negative breast cancer has a high rate of recurrence – or return – within the first three years after treatment, but then there’s a marked reduction after five years. Some factors may increase one’s risk of recurrence, such as being diagnosed at age 35 or younger, having a large tumor or cancer cells in the lymph nodes at the time of diagnosis or undergoing a lumpectomy without radiation therapy.
Moffitt Cancer Center’s approach to triple negative breast cancer
At Moffitt Cancer Center, we believe in a multispecialty approach to breast cancer diagnosis and treatment. Our Don & Erika Wallace Comprehensive Breast Program comprises highly specialized medical oncologists, radiologists, fellowship-trained surgeons, radiation oncologists and other health care professionals who work together to provide our patients with well-rounded care. Our patients also have access to our supportive care services, which include counseling, integrative medicine, nutritional help and much more.
We continue to make strides in developing our understanding of triple negative breast cancer. Treatments are being evaluated regularly by medical researchers and clinicians as more is being learned about triple negative cancers. Our extensive research efforts and innovative clinical trials help our patients lead healthy and productive lives.
If you are interested in learning more about triple negative breast cancer treatment at Moffitt, call 1-888-663-3488 or complete a new patient registration form online.
Breast Cancer Outcomes
The goal of any cancer treatment is to achieve the most favorable outcome while minimizing side effects and ensuring the best possible quality of life. On average, Moffitt's breast cancer treatment survival rates exceed 1.5 times the national average.
