Highlights of Moffitt Science Presented at Tandem Meetings of ASTCT and CIMBTR
Moffitt scientists are presenting advances in areas like cellular immunotherapy for relapsed or refractory (R/R) acute myeloid leukemia (AML), myelodysplastic syndromes (MDS), acute lymphoblastic leukemia (ALL), lymphoma, multiple myeloma (MM) and allogeneic HCT.
Featured abstracts:
- Phase I Trial of CD8-Depleted Human Leukocyte Antigen (HLA) Mismatched Unrelated Donor Lymphocyte Infusion (DLI) to Achieve Remissions in Myelodysplastic Syndrome (MDS) and Secondary Acute Myeloid Leukemia (sAML) (Elmariah et al., abstract #265). We here studied the HLA mismatched unrelated DLI as a novel cellular therapy to induce remission in patients with high-risk MDS and sAML. The treatment was safe and well tolerated in all study patients. Importantly, we observed dose-dependent response with 2/3 of patients at dose level 3 achieving complete remission. This promising therapy is now actively enrolling patients in an expansion cohort at Moffitt.
- Subgroup Analyses of Kte-X19, an Anti-CD19 Chimeric Antigen Receptor (CAR) T-Cell Therapy, in Adult Patients (Pts) with Relapsed/Refractory B-Cell Acute Lymphoblastic Leukemia (R/R B-ALL) in Zuma-3 (Shah et al., abstract #9). In this study of 78 adult patients with R/R B-ALL, the benefit to KTE-X19 was observed regardless of prior exposure to blinatumomab or prior allogeneic HCT. These findings highlight the effectiveness of KTE-X19 therapy in patients with heavily treated R/R B-ALL who have no available standard of care options.
- Association of Metabolic Tumor Volume (MTV) and Clinical Outcomes in Second-Line (2L) Relapsed/Refractory (R/R) Large B-Cell Lymphoma (LBCL) Following Axicabtagene Ciloleucel (Axi-Cel) Versus Standard-of-Care (SOC) Therapy in Zuma-7 (Locke et al., abstract #497). In this large analysis of patients with R/R LBCL, high MTV was associated with superior outcomes with axi-cel vs SOC therapy. High MTV vs low MTV influenced Grade ≥3 NEs and CRS with axi-cel. These findings suggest that MTV can be used as an accurate and sensitive measure of tumor burden in patients with R/R LBCL.
- Baseline Levels of Systemic Inflammatory Markers Interleukin 6 and Ferritin Are Associated with Toxicities and Progression-Free Survival in Multiple Myeloma Patients Treated with Idecabtagene Vicleucel (Hansen et al., abstract #256). In patients with R/R MM treated with commercial ide-cel, high levels of baseline ferritin or IL6 resulted in increased cytokine release syndrome (CRS) and inferior progression-free survival. Tailoring toxicity and therapeutic management to patient risk may mitigate morbidity and mortality.
- Idecabtagene Vicleucel Chimeric Antigen Receptor T-Cell Therapy for Relapsed/Refractory Multiple Myeloma with Renal Impairment: Real World Experience (Sidana/Hansen et al., abstract #42). In this multicenter observational study, we evaluated the real-world outcomes of R/R MM patients with renal impairment treated with standard of care ide-cel. We observed that treatment with ide-cel is feasible in patients with renal impairment with a comparable efficacy profile as patients without renal impairment. Safety was comparable with notable exception of higher prevalence of short-term high-grade cytopenias.
- Anti-BCMA CAR T-Cell Commercial Slot Allocation in Patients with Relapsed/Refractory Multiple Myeloma: Insights from a Single Center Experience (Castaneda et al., abstract #282). We report Moffitt experience in attempting to provide prioritization strategy and equitable commercial anti-BCMA CAR T cell manufacturing slot allocation using physician consensus. The median time from consultation to leukapheresis and from leukapheresis to CAR T cell infusion was 149.5 and 48 days, respectively. Exploring other models of resource allocation may help improve slot allocation to optimize CAR T cell production process.
- The Effect of Mycophenolate Mofetil Dose per Kilogram on Outcomes of Haploidentical Donor Peripheral Blood Stem Cell Transplant with Post-Transplant Cyclophosphamide (Elmariah et al., abstract #363). In this collaborative study between Moffitt and City of Hope, which included 417 haploidentical donor HCT the weight based MMF dose had no significant impact on clinical outcomes. These results raise the possibility that MMF may not be a critical component of the PTCy-based GVHD prophylaxis platform.
- Donor γδ T Cells Influence Immune Escape and Relapse of Acute Myeloid Leukemia (AML) after Allogeneic Hematopoietic Cell Transplantation (HCT) (Bejanyan et al., abstract #555). We analyze bone marrow samples of patients with AML before and after allogeneic HCT and found increased inhibitory receptor expression on donor γδ T cells of patients who relapsed after HCT. These findings highlight the role of γδ T cells in AML relapse control after HCT. Our ongoing phase 1/1b study is currently exploring the safety and effectiveness of ex vivo expanded donor γδ T cells for treatment of adverse risk AML after allogeneic HCT.
- Outpatient Treatment with Anti-Sars-Cov-2 Monoclonal Antibodies and Remdesivir for COVID19 Infections Demonstrates Encouraging Outcomes in Hematopoietic Stem Cell Transplant Recipients: A Single-Center Experience (Ionescu/Faramand et al., abstract #437). We examined the outcomes of HCT patients who presented to Moffitt with COVID-19 infection. Treatment with anti-SARS-CoV-2 monoclonal antibodies or Remdsevir in HCT recipients showed COVID-19 mortality rate of only 2.3%. Our findings support continued vigilance against COVID-19 with vaccinations, early testing for symptomatic patients and prompt outpatient therapy in mildly symptomatic HCT recipients.
- Developing Contemporary Survivorship Clinic for Recipients of Hematopoietic Cell Transplantation: A Single Center Experience (Mohty/Liu et al., abstract #490). We report here our successful experience in launching a contemporary HCT Survivorship Clinic at Moffitt. This consultative clinic model is staffed by dedicated advanced practice professional under supervision of faculty with expertise in BMT survivorship. Our survivorship clinic focuses on surveillance of late effects and general cancer screenings after allogeneic and autologous HCT with plans to expand to a broader population receiving other cellular therapies later in 2023.
If you are attending, we hope you'll stop by our booth #823 to learn more about Moffitt.
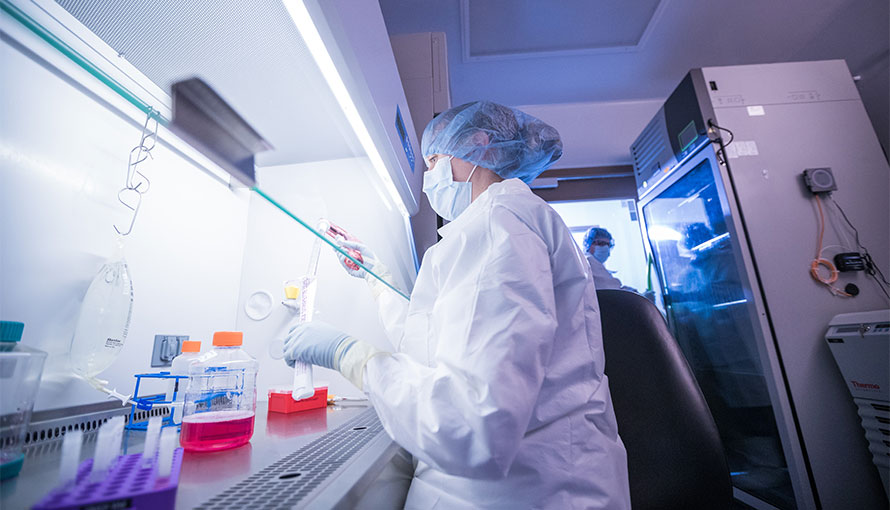
The largest transplant practice of its kind in the southeastern United States, Moffitt Cancer Center’s Blood and Marrow Transplant and Cellular Immunotherapy (BMT CI) Program provides patients with comprehensive diagnostic, donor matching, transplant as well as chimeric antigen receptor or CAR T cell therapy, other immunotherapy, and supportive care services in a single location.
If you'd like to refer a patient to Moffitt Cancer Center, complete our online form or contact a physician liaison for assistance. As part of our efforts to shorten referral times as much as possible, online referrals are typically responded to within 24 - 48 hours.
