Next-Gen Cell Therapy Shows Lasting Remission for Older Adults with Aggressive Leukemia
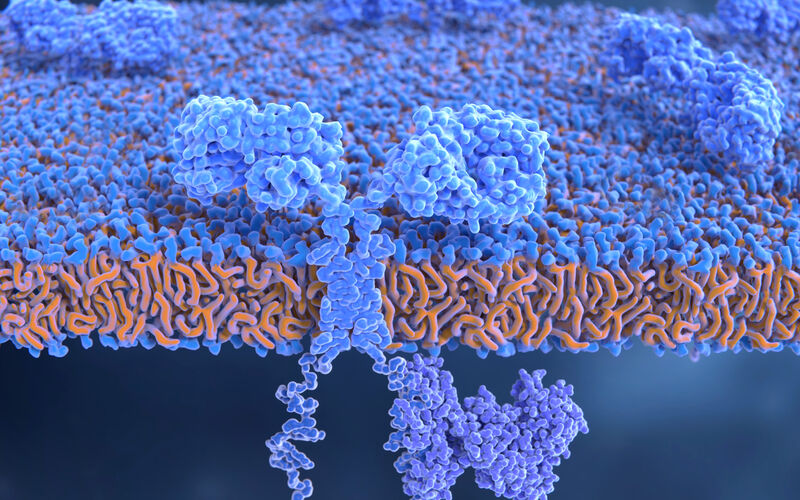
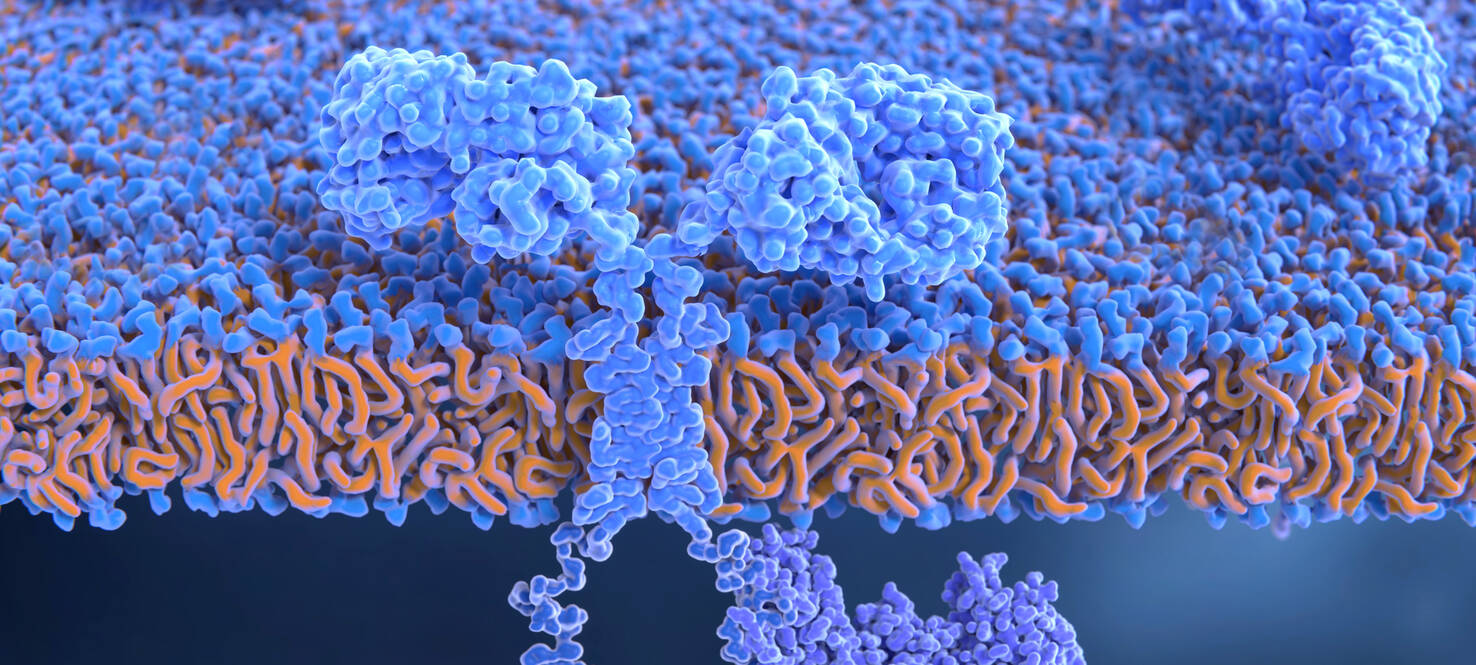
A recently approved cellular immunotherapy is continuing to change how doctors treat an aggressive type of leukemia, offering new options for patients who have relapsed or stopped responding to standard treatments. The therapy, called obecabtagene autoleucel, or obe-cel for short, is a chimeric antigen receptor T-cell (CAR T) therapy. It uses a patient’s own immune cells that are reprogrammed in a lab to recognize and destroy cancer cells.
Unlike traditional CAR T therapies, which typically use a single fixed dose, obe-cel takes a more individualized approach. The dose is tailored to the patient’s level of disease and delivered in two smaller infusions rather than one large one. This strategy appears to reduce the risk of severe immune-related side effects, which has made the treatment more accessible to patients who may not tolerate other CAR T options.
Now, new data from the FELIX trial presented at the 2025 European Hematology Association Congress show that obe-cel offers lasting results. The study included patients with relapsed or refractory B-cell acute lymphoblastic leukemia, a fast-growing cancer that is difficult to treat once it returns.

Bijal Shah, MD
Among patients who responded to therapy, the median duration of remission was more than three and a half years. More than half of patients remained in remission at 24 months, and 38.4% of responders did not need any additional treatment by month 33.
At 24 months, the probability of event-free survival was 43% and overall survival was 46%, suggesting many patients are not only staying in remission but also living longer. The study showed that obe-cel was effective across all age groups, particularly for those over 65.
“These updated results confirm what we’re already seeing in practice — that this therapy can meaningfully improve people’s lives, including for our more vulnerable older patients,” said Bijal Shah, MD, a medical oncologist in the Malignant Hematology Department at Moffitt Cancer Center. “Patients who previously had few options are achieving durable remissions, even without additional therapies like stem cell transplant.”
The study also found a few factors that were tied to better long-term outcomes. Patients were more likely to stay in remission if they had a certain genetic feature called Philadelphia chromosome-positive disease, started obe-cel treatment earlier, had less cancer in their body at the time of treatment or showed signs that the CAR T cells were still active in their system over time.
“These findings reinforce that we can make advanced therapies safer for a wider range of patients,” Shah said.