Radiation Therapy for Cervical Cancer

Cervical cancer develops in the cervix, the lower end of the uterus that opens into the vagina. Most cases begin with abnormal changes in the cervical lining, which progress gradually and become cancerous over time. If the changes are not detected early and treated, they can develop into invasive cancer, potentially spreading to surrounding tissues or distant parts of the body. Although cervical cancer can occur at any age, it is most frequently diagnosed in women in mid-adulthood, particularly between the ages of 35 and 55.
The primary cause of cervical cancer is a long-term infection with a high-risk strain of human papillomavirus (HPV), which is transmitted through sexual contact. Other contributing factors may include smoking, compromised immune function, multiple sexual partners or limited access to regular cervical cancer screenings. Because early-stage cervical cancer may not produce noticeable symptoms, routine Pap tests and HPV testing are essential for early detection.
When cervical cancer symptoms occur, they may include unusual vaginal bleeding or discharge, pelvic discomfort and pain during sexual intercourse. The diagnostic process typically begins with a pelvic examination and cervical cancer screening tests, which may be followed by medical imaging and a colposcopy or biopsy to confirm the diagnosis and assess how far the tumor has progressed. Cervical cancer is highly treatable when found early, but a delayed diagnosis can complicate treatment.
The best approach to cervical cancer treatment is determined by the type and stage of the tumor and the individual characteristics of the patient. While surgery can be effective for addressing an early-stage tumor, radiation therapy often plays a central role in treating more advanced cancer.
When is radiation therapy used for cervical cancer?
Radiation therapy is frequently used for cervical cancer, especially in cases where the tumor has spread beyond the cervix but has not yet reached distant organs or tissues. It may be used on its own or in combination with chemotherapy (chemoradiation) to target the cancer cells more aggressively.
Radiation therapy is often used after surgery to destroy any remaining microscopic cancer cells and help prevent recurrence. It can also be used as the primary treatment for cervical cancer if surgery is not an option due to the size or location of the tumor or the patient’s overall health condition.
What does radiation therapy for cervical cancer involve?
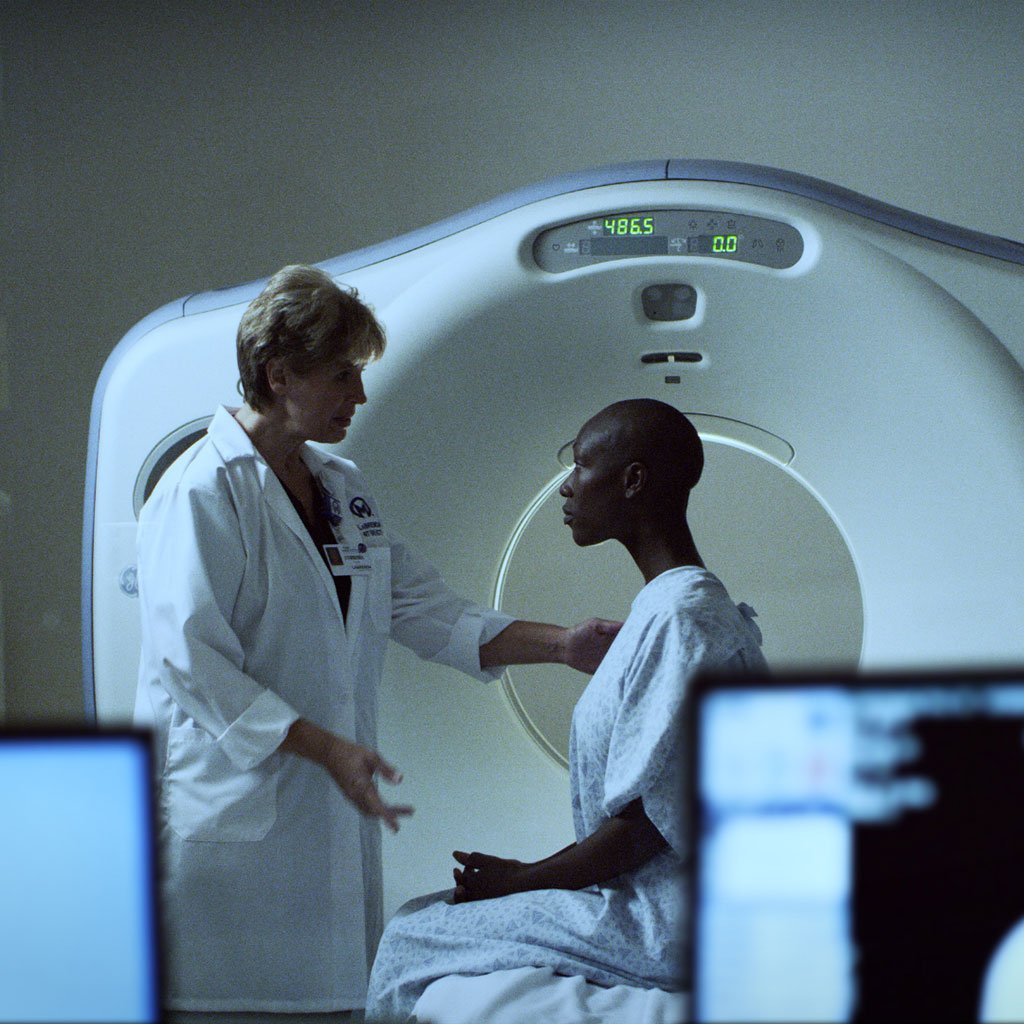
Radiation therapy uses high-energy rays to destroy cancerous cells or stop them from growing. Treatment for cervical cancer may involve a combination of external and internal radiation therapy. The physician will carefully plan treatment using imaging scans to ensure accurate targeting of the cancerous tissues are targeted accurately while minimizing any exposure to the surrounding healthy tissues.
External beam radiation therapy (EBRT) for cervical cancer
EBRT for cervical cancer involves the use of an external machine (linear accelerator) to deliver powerful radiation beams directly to the pelvis. By precisely targeting the tumor and affected lymph nodes, external beam radiation therapy can address both visible tumors and microscopic cancer spread. Usually, treatment is given five days a week over five to six weeks, often in combination with chemotherapy for enhanced treatment effectiveness. Each treatment lasts only a few minutes and is similar to undergoing a conventional X-ray, although the radiation dosage is higher.
What are the possible side effects of external beam radiation therapy for cervical cancer?
Common side effects of EBRT for cervical cancer include:
- Bladder irritation
- Diarrhea
- Fatigue
- Nausea
- Skin changes in the treated area
Some women also experience vaginal dryness or discomfort, especially toward the end of treatment. Usually, the side effects of EBRT are manageable with medications and lifestyle adjustments, and most resolve in the weeks following completion of therapy.
What are the risks and possible complications of external beam radiation therapy for cervical cancer?
In some cases, EBRT for cervical cancer may lead to long-term complications, such as:
- Chronic bladder or bowel problems
- Premature menopause
- Vaginal narrowing
Though rare, external radiation therapy for cervical cancer can sometimes damage the surrounding organs, such as the bladder or intestines, leading to persistent discomfort or bleeding. Careful treatment planning can minimize these risks, and the patient should promptly report any new or worsening symptoms to their healthcare team.

Ranked a Top Cancer Hospital in Nation
Moffitt is ranked 15th in the nation and is the top-ranked cancer hospital in Florida and the Southeast in Newsweek’s “America’s Best Cancer Hospitals."
What to expect during recovery from external beam radiation therapy for cervical cancer
Recovery from EBRT is gradual, and most short-term side effects improve within a few weeks after treatment is completed. The patient may continue to feel tired and require time to regain strength. Regular follow-up appointments will be necessary to monitor for any late-onset side effects and assess the treatment response. If needed, vaginal dilators and hormone therapy may be recommended to maintain tissue flexibility and manage menopausal symptoms.
How effective is external beam radiation therapy for cervical cancer?
EBRT can be effective in controlling cervical cancer, particularly when combined with chemotherapy. It can potentially shrink the tumor, eliminate any microscopic cancer cells that remain after surgery and reduce the risk of recurrence. In many cases of locally advanced disease, chemoradiation using EBRT can significantly improve the long-term outcome.
Internal radiation therapy for cervical cancer
Also known as brachytherapy, internal radiation therapy for cervical cancer uses a radioactive substance sealed within a special delivery device, which is carefully placed inside the body to deliver targeted radiation directly to the cervix and surrounding tissues. This treatment approach allows for a high dose of radiation to be focused precisely where it is needed, while limiting exposure to nearby healthy organs and tissues. Brachytherapy is commonly used after—or in combination with—EBRT. When treatment is complete, the device is removed from the body.
How is internal radiation therapy for cervical cancer delivered?
Brachytherapy is usually delivered in several sessions using a narrow applicator inserted into the vagina or cervix. The treatment may be administered as low-dose rate (LDR) therapy over several hours or high-dose rate (HDR) therapy in a shorter session lasting only a few minutes. Depending on the radiation delivery method, the patient may receive treatment as an outpatient or stay briefly in the hospital.
What are the possible side effects of internal radiation therapy for cervical cancer?
Common side effects of brachytherapy for cervical cancer include:
- Fatigue
- Pelvic cramping
- Temporary vaginal discomfort
Vaginal dryness, narrowing or soreness may develop over time, especially with repeated treatments. Some women also experience urinary or bowel changes in the days following treatment. These side effects are generally manageable and often improve with supportive care.
What are the risks and possible complications of internal radiation therapy for cervical cancer?
Though uncommon, brachytherapy can lead to long-term changes in vaginal tissues, bladder function or bowel habits. Rare complications include the development of scar tissue or fistulas between pelvic organs. The risk of complications increases with higher radiation doses and extended treatment, but the risk can be minimized with the use of precise imaging and careful planning.
What to expect during recovery from internal radiation therapy for cervical cancer
Recovery from brachytherapy is typically quicker than recovery from EBRT, but the patient may still experience temporary fatigue or pelvic discomfort. Over time, regular use of vaginal lubricants or dilators may be recommended to help prevent vaginal narrowing or tissue stiffening. Follow-up visits will be necessary to monitor for delayed side effects and evaluate the success of treatment.
How effective is internal radiation therapy for cervical cancer?
Brachytherapy has proven to be effective in targeting cervical tumors and minimizing cancer recurrence. When used alongside EBRT and chemotherapy, it can significantly increase the likelihood of long-term tumor control or cure in a patient with locally advanced cervical cancer. The precision of internal radiation therapy makes it a key component of modern cervical cancer treatment protocols.
Benefit from world-class care at Moffitt Cancer Center
Radiation therapy for cervical cancer is complex, and a key factor in its effectiveness is its delivery. Accredited by the American College of Radiology (ACR), Moffitt’s Radiation Oncology Program offers the latest radiation treatment techniques and technologies, including a robust portfolio of clinical trials. However, it is the expertise of our multispecialty team that truly sets us apart. We are also proud to be one of only a few cancer centers in the United States to offer ovarian transposition (oophoropexy) as a fertility-preservation option for cervical cancer patients.
If you would like to learn more about radiation therapy for cervical cancer, you can request an appointment with a specialist in our Gynecologic Oncology Program by calling 1-888-663-3488 or submitting a new patient registration form online. We do not require referrals.
New Brachytherapy Suite
The new brachytherapy suite at the Magnolia campus represents our commitment to innovation and excellence in patient care.
- Reduced Procedure Time – Cuts treatment time from ~10 hours to 5 hours per patient.
- Increased Capacity – Allows more patients to access timely, advanced care.
- Enhanced Safety – Reduces risks of applicator displacement with precise planning.
- Patient-Friendly Design – Provides a comfortable, sedated environment for recovery.
- Optimized Workflow – Spacious, well-equipped facilities improve efficiency.
- Improved Patient Care – Maintains high standards while reducing contact hours.
Radiation Therapy
