What is Follicular Lymphoma?

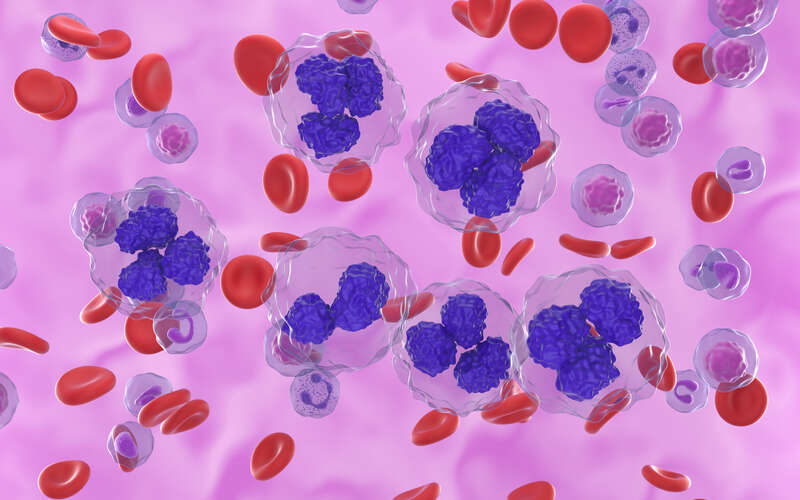
Follicular lymphoma is a slow-growing blood cancer that develops in the lymphatic system, a vast network of vessels and tissues that circulates lymph fluid and supports the body’s immune function. Because it arises in antibody-producing white blood cells (B lymphocytes), it is classified as a subtype of B-cell lymphoma. Unlike more aggressive hematologic cancers, follicular lymphoma may not produce noticeable symptoms for several years. Currently, there is no cure.
Although follicular lymphoma is a chronic and typically manageable type of non-Hodgkin lymphoma, a timely diagnosis and ongoing monitoring are essential to guide treatment planning and maintain quality of life.
What are the warning signs and symptoms of follicular lymphoma?
In many cases, the first sign of follicular lymphoma is painless swelling of the lymph nodes, most often in the neck, armpits or groin. Some patients may also experience:
- Abdominal discomfort or fullness caused by lymph node or spleen enlargement
- “B symptoms,” which include fever, drenching night sweats and unintended weight loss
- Frequent infections due to reduced immune function
- Persistent fatigue or lack of energy
-
1 out of 5
lymphomas in the U.S. is follicular lymphoma
-
About 60
average age of diagnosis
What are the causes and risk factors for follicular lymphoma?
The exact cause of follicular lymphoma is not fully understood. Researchers have linked many cases to an uninherited genetic mutation known as the t(14;18) translocation, which occurs in certain B lymphocytes sometime during the patient’s lifetime. This acquired DNA change causes the BCL2 gene—which is responsible for regulating cell death—to become overactive and produce too much BCL2 protein. As a result, abnormal B cells live longer than they should and begin to accumulate in the lymph nodes, which can lead to follicular lymphoma.
In addition to the t(14;18) translocation, several other factors may increase the risk of developing follicular lymphoma. These include:
- Advanced age – Most cases are diagnosed in adults 60 and older.
- Certain environmental exposures – Long-term contact with harmful chemicals, such as pesticides, herbicides and solvents, can increase the risk.
- Certain infections – Infections that chronically stimulate the immune system may play a role in the development of follicular lymphoma, although no single infectious cause has been confirmed.
- Family history – Having a close relative with non-Hodgkin lymphoma or another blood cancer may raise the risk.
- Female gender – Follicular lymphoma affects slightly more women than men. The reason is unknown.
- Weakened immune system – Individuals who are immunocompromised due to a human immunodeficiency virus (HIV) infection, an autoimmune disorder or immunosuppressive medications may be at heightened risk.


Rated High Performing in Leukemia, Lymphoma & Myeloma
Schedule an AppointmentHow is follicular lymphoma diagnosed?
Diagnosing follicular lymphoma usually requires a series of steps that allow the physician to confirm the presence of cancer and understand its specific features. This process may include:
- Clinical assessment – After reviewing the patient’s symptoms, medical history and risk factors, the physician will typically perform a physical examination, specifically checking for signs of lymph node, spleen or liver enlargement.
- Lymph node biopsy – This procedure involves removing all or part of an enlarged lymph node for microscopic examination by a pathologist, who can confirm the presence of lymphoma and characterize its specific features.
- Laboratory tests – The physician may order a complete blood count (CBC) to measure the levels of red blood cells, white blood cells and platelets in the bloodstream, and other lab tests to assess liver and kidney function.
- Imaging studies – Computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET) scans can help the physician evaluate the location and size of the affected lymph nodes and identify possible signs of cancer in other areas of the body.
- Bone marrow biopsy – To determine whether follicular lymphoma has spread to blood-forming tissues, the physician may take a sample of bone marrow (usually from the hip bone) for microscopic examination by a pathologist.
- Molecular and genetic testing – In some cases, biopsy samples may be tested for genetic changes, such as the t(14;18) translocation, which is common in follicular lymphoma.
How is follicular lymphoma staged?
Once a diagnosis of follicular lymphoma is confirmed, the physician will determine the stage of the cancer to assess how far it has spread in the body. Staging helps guide treatment planning and provides important information about prognosis. The Ann Arbor staging system is the standard classification method used for both Hodgkin and non-Hodgkin lymphoma. The stages of follicular lymphoma include:
- Stage 1 – Cancer is found in a one lymph node region or lymphoid structure, such as the spleen or thymus, or a single site outside the lymphatic system.
- Stage 2 – Cancer is found in two or more lymph node regions on the same side of the diaphragm, and possibly one nearby organ or tissue.
- Stage 3 – Cancer is found in lymph node regions on both sides of the diaphragm, and possibly the spleen or a nearby organ.
- Stage 4 – Cancer has spread widely to one or more tissues or organs outside the lymphatic system, such as the bone marrow, liver or lungs.
Based on the patient’s symptoms, the letter A or B may be added to the numeric follicular lymphoma stage as follows:
- A – No significant systemic symptoms are present.
- B – The patient is experiencing B symptoms.
How is follicular lymphoma treated?
Follicular lymphoma treatment is tailored to the patient’s symptoms and overall health. Treatment options may include:
Active surveillance (watchful waiting)
If follicular lymphoma is found to be slow-growing and not causing symptoms, the physician may recommend regular checkups, blood tests and imaging scans rather than beginning treatment immediately. This watchful waiting approach can allow the patient to avoid unnecessary therapy and potential side effects, while ensuring that treatment can begin promptly if the cancer shows signs of progression.
Targeted therapy
Targeted therapies, such as rituximab, are medicines that attach to specific proteins on lymphoma cells. This can help the immune system find and destroy the cancer cells while leaving most healthy cells unharmed. For this reason, targeted therapy often causes fewer side effects than traditional treatments.
Chemotherapy
Chemotherapy uses a customized regimen of powerful medications to destroy rapidly dividing cells, including cancer cells, or stop them from dividing. Typically, chemo drugs are given in cycles, with each period of active treatment followed by a period of rest to allow the body time to recover. To address follicular lymphoma, chemo may be combined with targeted therapy for heightened treatment effectiveness.
Radiation therapy
Radiation therapy delivers high-energy beams to a precise area of the body affected by cancer. This treatment approach is generally most effective for early-stage follicular lymphoma that is confined to one or two lymph node regions.
Immunotherapy
The goal of immunotherapy is to bolster the natural ability of the body’s immune system, helping it to attack cancer cells more effectively. For follicular lymphoma, options may include immune checkpoint inhibitors and CAR T-cell therapy, which uses the patient’s own modified immune cells to target lymphoma cells.
Additionally, in July 2024, the U.S. Food and Drug Administration (FDA) approved epcoritamab, an immunotherapy specifically designed to address relapsed and refractory follicular lymphoma. This bispecific antibody is designed to bind to two different antigens simultaneously, allowing it to engage two different targets: proteins on T cells and proteins on follicular lymphoma cells. By latching onto both types of proteins, epcoritamab can guide the T cells directly to the cancer cells. This highly targeted treatment approach can allow the immune system to destroy follicular lymphoma cells more precisely.


#1 Cancer Hospital in Florida
Schedule an AppointmentBone marrow transplantation
During a bone marrow transplant, the patient’s damaged bone marrow is replaced with healthy blood-forming cells, which may be derived either from the patient’s own body or a compatible donor. This intensive treatment is usually reserved for recurrent or difficult-to-treat follicular lymphoma.
Clinical trials
Clinical studies offer some patients unique opportunities to be among the first to benefit from promising new treatments—such as advanced targeted drugs, cancer vaccines and novel cell therapies—before those options are made widely available in other settings.
Benefit from world-class care at Moffitt Cancer Center
For the diagnosis and treatment of follicular lymphoma, many patients confidently turn to Moffitt. The multispecialty team in our renowned Malignant Hematology Program includes numerous follicular lymphoma specialists, such as surgeons, medical oncologists, radiation oncologists, radiologists, nurses and supportive care providers. Working together, we help each patient achieve the best possible outcome and quality of life.
To request an appointment with a specialist on our team, call 1-888-663-3488 or complete our new patient registration form online. We do not require referrals.
References
Non-Hodgkin Lymphoma Stages
Follicular Lymphoma | Non-Hodgkin Lymphoma | Cancer Research UK
Follicular Lymphoma
Follicular Lymphoma - NORD (National Organization for Rare Disorders)
Follicular Lymphoma