Whipple Procedure for Pancreatic Cancer Treatment
The Whipple procedure, also known as a pancreaticoduodenectomy, is the most common type of pancreatic cancer surgery. The goal is to remove a localized tumor from the head of the pancreas. This complex procedure is named after Dr. Allen O. Whipple, the first surgeon to perform a two-stage resection of the first part of the small intestine (duodenum) and head of the pancreas in 1935.
By 1940, Dr. Whipple had refined the technique into a single-stage procedure, establishing what would become the standard surgical approach for removing pancreatic tumors. Since then, advancements in surgical methods and postoperative care have significantly improved the outcome and quality of life for many pancreatic cancer patients.
What does a Whipple procedure for pancreatic cancer treatment involve?
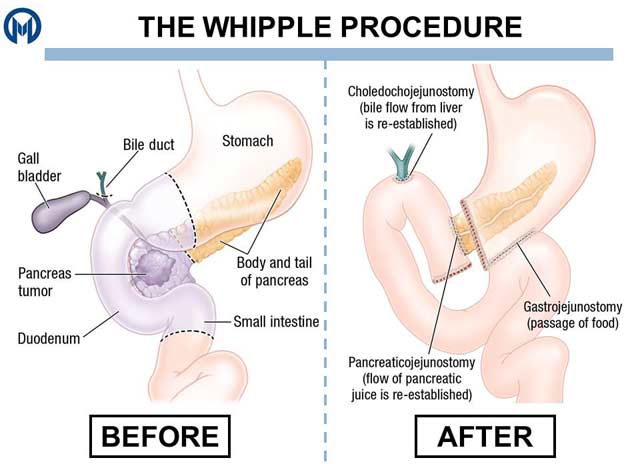
A standard Whipple procedure involves surgically removing:
- The head of the pancreas (approximately 50% of the organ)
- The duodenum
- The gallbladder
- Part of the common bile duct
- The surrounding lymph nodes
- Approximately 10% of the stomach
- Sections of nearby blood vessels
The primary goal of this intricate surgery is to remove the entire tumor along with nearby lymph nodes where cancer cells may have spread. The surgeon will then reconnect the pancreas, common bile duct and small intestine to restore digestive function.
In some cases, the surgeon may utilize a modified surgical approach known as a pylorus-preserving Whipple procedure. This method involves preserving the entire stomach and stomach valve (pylorus) when removing the tumor and other affected structures.
What happens during a Whipple procedure for pancreatic cancer treatment?
Before undergoing Whipple surgery, the patient will receive general anesthesia to ensure they remain asleep throughout the procedure, which typically takes five to seven hours to complete. Whipple surgery can be performed using traditional or minimally invasive robotic-assisted surgical techniques.


Rated High Performing in Gastrointestinal Cancer Surgery
Schedule an AppointmentTraditional Whipple procedure for pancreatic cancer treatment
When performing traditional open Whipple surgery for pancreatic cancer, the surgeon will make a large incision in the abdomen to access, remove and reconstruct the pancreas and other organs and structures affected by the cancer.
Robotic Whipple procedure for pancreatic cancer treatment
When performing minimally invasive robotic-assisted Whipple surgery, the surgeon will make several small incisions in the abdomen and complete the procedure using advanced robotic technology, such as the da Vinci® Surgical System.
The da Vinci® Surgical System incorporates several innovative features that will allow the surgeon to make smaller, more precise movements during surgery. These features include:
- A high-definition visualization system that will provide the surgeon with highly magnified, three-dimensional (3D) views while operating
- Wristed surgical instruments that can rotate and bend far beyond the capabilities of the human hand
- Robotic technology that will translate the surgeon’s hand movements into smaller, more precise actions
Who performs the Whipple procedure for pancreatic cancer treatment?
The Whipple procedure is one of the most complex surgeries performed for pancreatic cancer treatment. Due to its technical difficulty and potential for complications, it requires a highly trained, multidisciplinary medical team working together before, during and after the surgery. Key roles include:
Surgical oncologist or hepatopancreatobiliary (HPB) surgeon
The lead surgeon—often a surgical oncologist or HPB surgeon—is responsible for performing the Whipple procedure. This specialist has extensive expertise in operating on the pancreas, bile ducts, liver and surrounding organs. After carefully removing the affected section of the pancreas, nearby lymph nodes and portions of the bile ducts, small intestine and stomach if needed, the lead surgeon will reconstruct the digestive tract to restore normal function.


#1 Cancer Hospital in Florida
Schedule an AppointmentAnesthesiologist
Throughout the several-hour Whipple procedure, an experienced anesthesiologist will closely oversee the patient’s anesthesia, ensuring they remain safely sedated, stable and pain-free. This specialist will continually monitor the patient’s vital signs—including heart rate, blood pressure and blood-oxygen level—and make real-time adjustments to the anesthesia as needed.
Gastroenterologist
A gastroenterologist will help prepare the patient for Whipple surgery by performing vital diagnostic tests, such as endoscopic ultrasound (EUS) or endoscopic retrograde cholangiopancreatography (ERCP), to locate and evaluate the tumor. After surgery, the gastroenterologist may help monitor the patient’s digestive function and address any issues related to nutrient absorption or bile flow.
Oncologist
A medical oncologist will oversee any chemotherapy or other systemic treatments administered before or after surgery. For instance, the patient may receive chemotherapy before surgery to shrink the tumor and make it easier to remove, or after surgery to target any remaining cancer cells and help reduce the risk of recurrence. This specialist will monitor the patient’s response to systemic treatment and help manage any side effects.
Radiologist
A radiologist will play an essential role in the diagnostic and surgical planning phases. Using advanced imaging technologies, such as computed tomography (CT), magnetic resonance imaging (MRI and positron emission tomography (PET) scans, the radiologist will help determine the location, size and spread of the tumor and assess whether it can be safely removed. During recovery, the radiologist may also perform follow-up imaging tests to monitor the patient’s healing and check for any signs of recurrence or complications.
Pathologist
A pathologist will be responsible for analyzing tissue samples taken during the Whipple procedure. By examining the excised tissue under a microscope, the pathologist can confirm the diagnosis, identify the cancer type and determine whether all cancerous cells have been removed (“clear margins”). These findings will be critical for guiding further treatment decisions, such as whether follow-up chemotherapy or radiation therapy is necessary.
Nutritionist
A nutritionist will help the patient adapt to any necessary dietary changes following the Whipple procedure. Because the surgery alters the digestive system, the patient may have difficulty digesting or absorbing nutrients. The nutritionist can provide a customized eating plan that supports healing, minimizes digestive discomfort and helps the patient maintain strength and weight during recovery.
Rehabilitation and nursing team
A dedicated rehabilitation team, including physical therapists, occupational therapists and specialized nurses, will help the patient regain strength and mobility after Whipple surgery. These specialists can provide individualized guidance on safe movement, exercise and daily activities during recovery. Nurses will also provide wound care, pain management and ongoing monitoring of the patient’s recovery progress.
Together, this multidisciplinary team will ensure that each stage of the patient’s pancreatic cancer care—from diagnosis and surgery to recovery and long-term management—is comprehensive and well-coordinated. For a patient undergoing Whipple surgery, this collaborative approach can improve the surgical outcome and support a smooth recovery.
What are the risks and possible complications of a Whipple procedure for pancreatic cancer treatment?
The Whipple procedure for pancreatic cancer is a complex and extensive surgery that carries several risks and potential complications, including:
- Infection – As with any major surgery, there is a risk of infection at the incision site.
- Excessive bleeding – Significant blood loss can occur during or after the procedure.
- Delayed gastric emptying – After surgery, the stomach may empty its contents more slowly, which can cause nausea and vomiting.
- Pancreatic fistula – Leakage from the surgical connections can lead to the formation of an abnormal connection between the pancreas and another organ.
- Nutritional deficiencies – Difficulty digesting food and absorbing nutrients can result in weight loss and malnutrition.
- Diabetes – Removal of part of the pancreas can affect insulin production, potentially leading to diabetes.
The risk level can vary depending on the patient’s overall health and other individual factors. To help the patient make fully informed treatment decisions, the surgeon will fully explain the risks and possible complications of the Whipple procedure for pancreatic cancer.
What to expect during recovery from a Whipple procedure for pancreatic cancer treatment
After undergoing Whipple surgery, the patient will remain in the hospital for one to two weeks, allowing the medical team to closely monitor for signs of surgical complications, such as infection, bleeding and digestive issues. During the first few days, the patient will be restricted from eating solid foods as the digestive system begins to heal. Until the patient can safely tolerate liquids and soft foods, nutrition may be provided through an intravenous (IV) or feeding tube.
Continuing recovery and follow-up
Before the patient is discharged home, the surgical team will provide detailed instructions on wound care, activity restrictions, dietary guidelines and follow-up appointments. Ongoing monitoring will help ensure the pancreas and digestive system are functioning properly and the patient continues to recover as expected.
Pain management
Early in the recovery process, some pain around the incision site is normal. The surgical team will provide pain medication and guidance on how to manage any discomfort at home. The patient should take their medications as directed and communicate with the physician about any changes in pain levels or new symptoms.
Dietary adjustments
After Whipple surgery, the patient will need to reintroduce foods slowly to give their digestive system time to adjust to the anatomical changes. The surgeon or dietitian will provide a detailed plan outlining which foods to start with and how to transition to a more normal diet. The patient may need to eat smaller, more frequent meals and avoid fatty or greasy foods. Enzyme supplements may also be prescribed to aid digestion, especially if the pancreas is not producing enough digestive enzymes.
Potential side effects and complications
Some patients may experience digestive changes, such as nausea, bloating, diarrhea or malabsorption. Weight loss is also common in the early stages of recovery. More serious complications—such as infection, leakage at a surgical connection and delayed gastric emptying—require immediate medical attention. Regular follow-up visits can allow the medical team to monitor the patient’s healing progress and address any concerns early.
Recovery time and physical healing
Full recovery from a Whipple procedure typically takes six to eight weeks, although it can take up to several months for the patient to regain their normal strength and energy levels. Fatigue is common, and light activities should be gradually reintroduced as recommended by the surgeon. Over time, the patient should notice steady improvements in their stamina and appetite.
How effective is the Whipple procedure for pancreatic cancer treatment?
Whipple surgery can be highly effective for pancreatic cancer, particularly when the tumor is located in the head of the pancreas and has not spread extensively. When performed by an experienced surgeon at a high-volume cancer center, the procedure often leads to an excellent outcome and sometimes a cure. That said, its effectiveness can vary based on factors such as the stage of the tumor, the completeness of its removal and the patient’s overall health.
What are some frequently asked questions (FAQs) about the Whipple procedure for pancreatic cancer treatment?
The prospect of Whipple surgery can be daunting, and many patients understandably have questions about what to expect before, during and after the procedure. While the best source of information is always the patient’s own medical team, these general answers to some frequently asked questions might be helpful:
What types of cancer can be treated with Whipple surgery?
The Whipple procedure is primarily used to treat pancreatic cancer located in the head of the pancreas, but it can also be an effective surgical option for several other conditions affecting nearby organs. These include:
- Ampullary cancer, which forms where the bile duct and pancreatic duct meet
- Distal bile duct cancer
- Duodenal cancer, which occurs in the first part of the small intestine
- Neuroendocrine tumors of the pancreas
In some cases, the Whipple procedure may also be performed to remove a benign pancreatic tumor or precancerous cyst that has a high risk of becoming malignant. By removing the affected portions of the pancreas, bile duct and small intestine, Whipple surgery can help eliminate or control cancer confined to this region of the body before it spreads.
How long does a Whipple procedure take to complete?
Whipple surgery is a highly complex procedure that typically takes five to seven hours to complete. The duration of the surgical session can vary depending on the extent of the cancer and whether any nearby organs or other tissues are affected.
What can I eat after Whipple surgery?
Initially, most patients are limited to clear liquids before slowly transitioning to soft foods and then small, frequent meals. A low-fat, high-protein diet is generally recommended, along with plenty of fluids.
A nutritionist can help the patient identify foods that are easy to digest and may suggest enzyme supplements if appropriate. To minimize digestive discomfort, the patient should avoid greasy, fried and sugary foods.
Will I lose weight after Whipple surgery?
Weight loss is common after the Whipple procedure, mainly because the surgery affects how the body digests and absorbs nutrients. This can lead to reduced appetite, changes in digestive function and difficulty maintaining weight. With time and dietary adjustments overseen by a nutritionist, most patients can regain some of the weight lost after surgery.
Will I need chemotherapy or radiation therapy after Whipple surgery?
Many patients receive chemotherapy or radiation therapy after Whipple surgery to help destroy any remaining cancer cells and reduce the risk of recurrence. A medical oncologist will review the pathology results and recommend a personalized treatment plan based on the type and stage of the tumor.
When should I call my physician after Whipple surgery?
The patient should contact their physician right away if they experience:
- Persistent fever or chills
- Worsening abdominal pain or swelling
- Signs of infection, such as redness, drainage or warmth around the incision site
- Difficulty eating or digesting food
- Sudden weight loss
- Severe fatigue
Early intervention can help prevent complications and ensure the best recovery outcome.
Does Whipple surgery offer a cure for pancreatic cancer?
In many cases, the Whipple procedure offers the best chance for long-term survival and a potential cure for pancreatic cancer, but it is not suitable for all patients. This intensive surgery is typically recommended only when the cancer is confined to the head of the pancreas and has not spread to major blood vessels or distant organs. If the entire tumor can be successfully removed with clear margins, the likelihood of long-term remission improves significantly. However, because pancreatic cancer can be aggressive and may return even after surgery, most patients also receive chemotherapy or radiation therapy following the Whipple procedure to reduce the risk of recurrence and improve the overall outcome.
Benefit from world-class care at Moffitt Cancer Center
Moffitt is a high-volume cancer center, and this translates to extensive experience in pancreatic cancer treatment. To date, our multispecialty team has completed more than 2,000 Whipple procedures, a complex surgery that demands highly refined expertise. We also have a robust portfolio of clinical trials, which provides our patients with unique opportunities to be among the first to benefit from promising new therapies that are not yet available in other settings.
If you would like to learn more about the Whipple procedure for pancreatic cancer, you can request an appointment with a specialist in our Gastrointestinal Oncology Program by calling 1-888-663-3488 or submitting a new patient registration form online. We do not require referrals.
Helpful links: