Advocating for Patients From Bench to Bedside
At Moffitt Cancer Center, physicians and scientists are dedicated to patient-centered care. Each patient is unique, with their own needs, priorities and journeys. Some have taken a long and winding road to get to a diagnosis. Many face tough life-altering decisions about their treatment. These lived experiences influence how oncologists care for the patients of today and how researchers improve care for the patients of tomorrow.
Across Moffitt, women physicians and researchers are advocating for patients in a variety of ways. They’re educating fellow physicians on rare diseases, incorporating patient perspectives into scientific analysis and helping patients find their voice through difficult conversations. This commitment to prioritizing the patient perspective drives compassionate care in the clinic and fosters insightful research from the field. Most importantly, it leads to improved outcomes for patients.
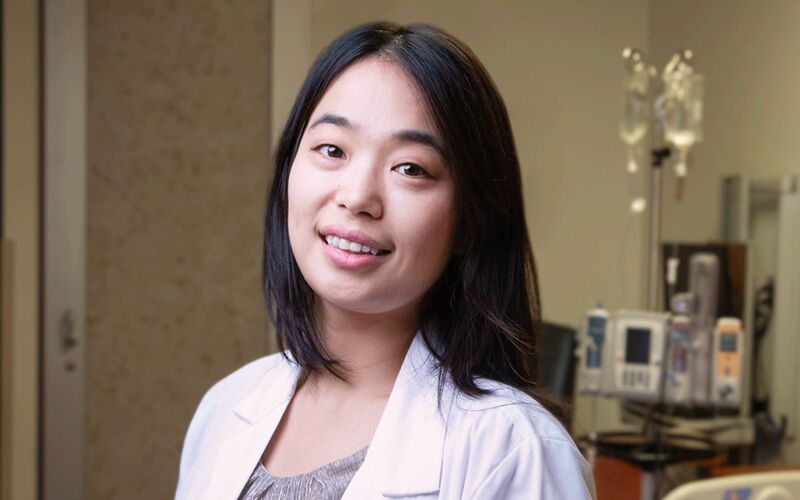
Representing Patients With Rare Diseases
When patients finally reach Yumeng Zhang, MD, many have already endured a long and frustrating journey, often spending nearly a decade in search of a diagnosis. As an oncologist in the Malignant Hematology Department at Moffitt, Zhang focuses on cutaneous T-cell lymphoma (CTCL), rare cancers that are often misdiagnosed as more common skin conditions like eczema. These patients suffer from debilitating symptoms: intense itching, painful rashes and, in some cases, visible tumors and skin ulcers.
By the time they find their way to Zhang, most of these patients have become their own advocates, forced to navigate a fragmented health care system that has failed to provide answers. In one instance, a patient tracked Zhang down at the World Congress of Cutaneous Lymphomas, an event typically attended by oncologists, while relentlessly searching for solutions to their own rare disease.
“This is a group of patients who are often the most forgotten in the medical system,” Zhang explained. “They need help more than most, and their fight for recognition and proper care is ongoing.”
The challenges faced by patients with rare diseases like CTCL extend well beyond the difficulties of getting a diagnosis. Treatment options are limited, and opportunities for clinical research are scarce. Many patients must travel significant distances to access specialized care at centers like Moffitt. For those who have exhausted first-line treatments without success, the task of finding a clinical trial feels overwhelming. In fact, Moffitt is the only center in Florida offering a clinical trial specifically for CTCL, highlighting the stark reality for these patients.
To address these gaps in care, Zhang employs a comprehensive approach that blends education, collaboration and systemic change. She regularly meets with dermatologists, both in person and virtually, to raise awareness of CTCL and ensure that these rare cancers are recognized and treated appropriately. Additionally, she works closely with patients’ local care teams — dermatologists, oncologists and wound care specialists — personally reaching out to ensure that everyone involved understands the disease and treatment plan.

“Doctors should always teach patients how to advocate for themselves,” Zhang said. “But as a medical community, we must take the initiative to reach out as well. By sharing knowledge, we widen the circle of care and ensure more patients benefit.”
Zhang and her team are also pioneering innovative clinical trial designs to overcome the challenges specific to rare diseases. Given the small number of patients available for such studies and the difficulties of traveling long distances to participate, they are exploring new models. This includes using larger population data sets as control groups and decentralizing trials to allow patients to participate from home through telemedicine and remote monitoring.
Ultimately, Zhang believes that advocating for patients with rare diseases has far-reaching implications for the entire health care system.
“Patients with rare diseases are among the most vulnerable in health care. If we can dismantle the barriers they face — whether financial, related to clinical trial design or securing research funding — we’re not just improving care for them. We are removing systemic obstacles for everyone. Each problem we solve for these patients leads to solutions that benefit all.”
Zhang’s work is rooted in urgency and deep compassion. She knows that advocating for patients with rare diseases isn’t just about offering better treatments — it’s about ensuring that the most overlooked members of the health care system are seen, heard and cared for. It is a fight for their right to equitable care, and in doing so, it is a fight for the future of health care for everyone.
Incorporating Patient Voices Into Research
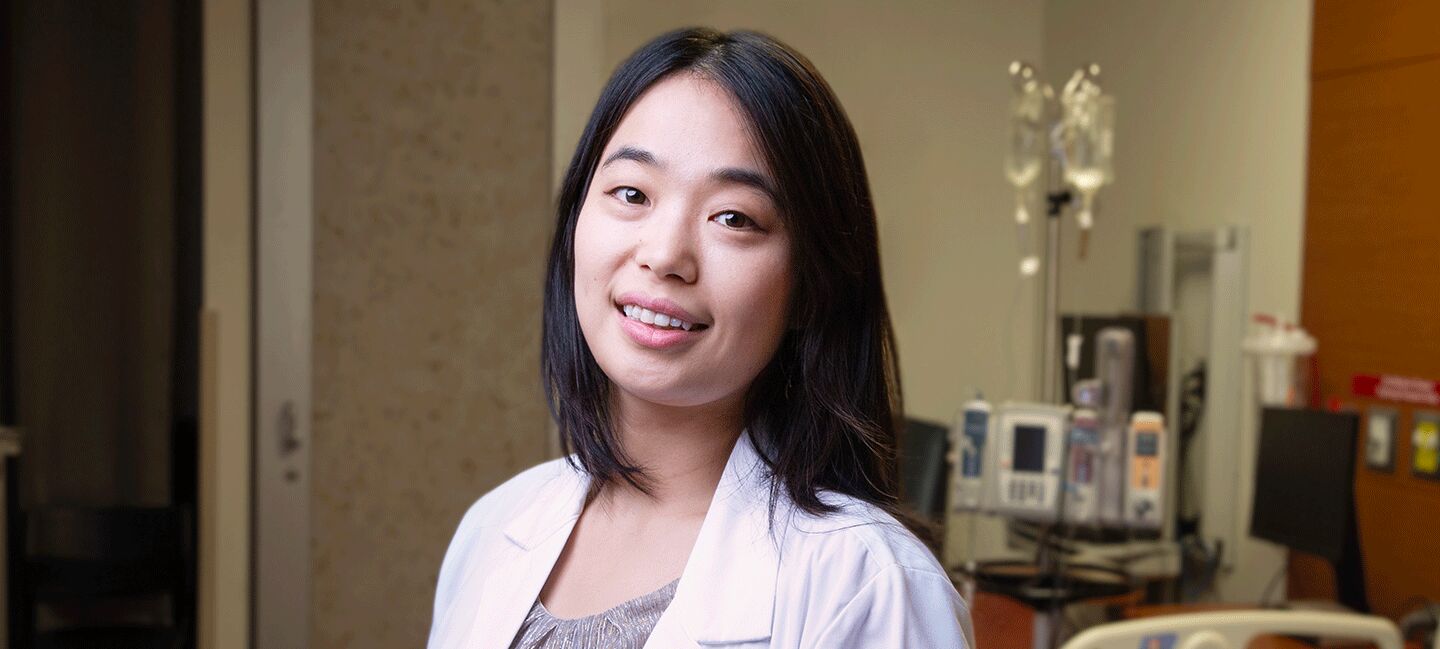
Cancer epidemiologist Jessica Islam, PhD, focuses her research on improving and optimizing care to marginalized populations, specifically people living with HIV. As treatments for HIV have improved over the years, people are living longer and beginning to experience the comorbidities associated with aging, including cancer.
Due to their HIV status, these patients often already have extensive experience with the health care system. These experiences can inform how they approach cancer care. Data shows that 1 in 4 people living with HIV do not receive cancer treatment after a cancer diagnosis. But the data doesn’t explain why.

Incorporating patient voices into research helps scientists like Jessica Islam, PhD, better understand the data they are collecting.
“Patient voices in this context are critical because they have a PhD in their lived experience. They know what are the issues that they experience on a day-to-day basis,” Islam said. “They are the ones who know how to improve feasibility, acceptability, rigor and relevance of the different research questions that we as scientists are asking.”
To highlight the salience of patient voices in research, Moffitt hosts regular forums focused on specific cancer sites or demographics. At these forums, scientists can directly hear from the patients they are trying to help. They can learn about patient concerns and hear the questions that are on patients’ minds.
In her research, Islam also partners with community organizations such as CAN Community Health, a network of clinics that serves people living with HIV and those who are at risk, to inform her research and gain community-level perspectives. Partnerships like this help Moffitt researchers connect with the populations they are studying through a trusted community group.
“Meeting people where they are is critical to addressing disparities,” Islam said. “They have lived experience that we as researchers simply don’t have, and that lived experience is vital to doing good science.”
Incorporating patient advocacy into research can then help shape how doctors care for patients in the clinic. For patients living with HIV and a cancer diagnosis, Islam stressed that it’s crucial for providers to understand the patient’s journey and how past interactions with the health care system affect how they approach cancer treatment. For marginalized populations overall, it’s important that doctors understand unique barriers to care and help ensure that supports like social services are in place to address those barriers.
“Patient advocacy really extends from the bench and goes all the way through to the clinic,” Islam said.
‘Defining the Right Care for a Patient’
Patient voices are central to the work of Sahana Rajasekhara, MD. As a palliative care physician, Rajasekhara supports patients through all stages of their cancer journey, from diagnosis and treatment to end-of-life decisions.
“Defining the right care for a patient goes beyond medical facts,” she explained. “It requires an understanding of patients’ personal values, needs and preferences in relation to the proposed cancer treatment.”
This collaborative approach, where patients and clinicians work together to determine the best course of care, is key to delivering the “right care” for everyone. For some, this might mean pursuing the most aggressive treatment with the hope for a cure. For others, it could mean prioritizing the best supportive care with a focus on quality of life. Providing patients with information they need to advocate for themselves is crucial.

Sahana Rajasekhara, MD, notes that it is crucial to understand patients’ needs, values and preferences to determine the right path forward.
“As providers, our role is to give patients the necessary information regarding their treatment options — risks, benefits and potential outcomes — and help them understand and navigate their choices,” Rajasekhara said.
By having these discussions, patients can select the treatment plan that best fits them, their values and needs. This shared decision-making ensures patients have a voice in their care and that the care is right for them. While these conversations can be difficult for both the providers and the patients, they are necessary. And they must be ongoing to reflect the changing needs of the patient.
As a program co-lead for Moffitt’s Improving Goal Concordant Care Initiative, a formal communication skill training program launched two years ago with high-level institutional support, Rajasekhara focuses on equipping providers to navigate serious illness conversations through both formal and informal training programs.
“This empowers providers to engage in timely, honest and empathetic conversations,” she explained. “It ensures that patients’ voices are heard, and their treatment plans reflect those choices — the right care for that patient. Advocating for patients is a cornerstone of quality health care, and through our collaborative efforts, we can ensure patients feel empowered to make informed decisions about their care.”
A Broad Impact
From individual patient conversations to innovative research, Moffitt is setting the standard for personalized, patient-centered care. As Rajasekhara put it:
“You have to empower patients and reinforce the idea that they’re the most important member of their health care team. It’s not the oncologist, it’s not the surgeon. The most important member of the health care team are the patients themselves.”