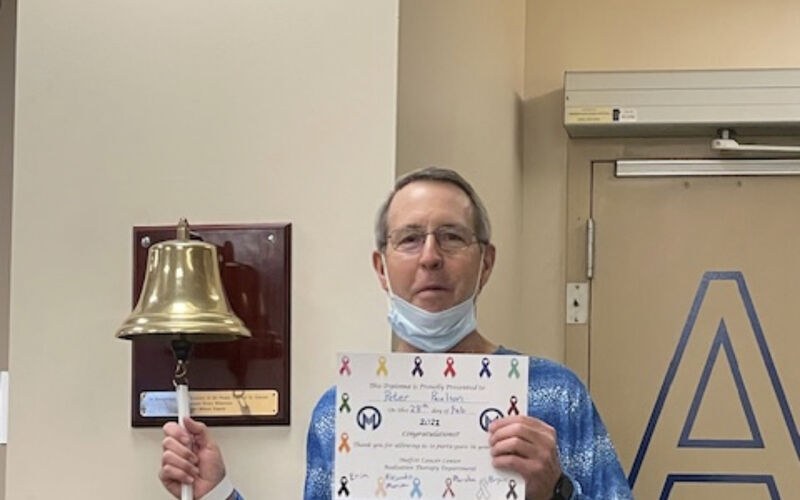
Clinical Trial Uses Personalized Radiation To Treat Rectal Cancer
A day out on the water, offshore fishing in the Florida sunshine, is 72-year-old Peter Paulson’s favorite way to spend his free time.
After being misdiagnosed as having hemorrhoids, Paulson learned he actually had stage 3 rectal cancer. That’s when he was referred to Moffitt Cancer Center.
Before beginning treatment, Paulson had a goal: to try his best to maintain his quality of life. At the time, Paulson met the criteria and enrolled in a rectal cancer clinical trial at Moffitt. The aim of the trial was for patients to receive treatment and avoid invasive surgery that could alter their quality of life.
Rectal surgery can impact a patient’s bowel and urinary functions and result in the need for a colostomy bag.
After his cancer diagnosis, Peter Paulson was determined to maintain his active lifestyle, including continuing to take offshore fishing trips.
“As a very active person, I can’t imagine how that could not have seriously compromised my way of life, so if there was any chance of avoiding that, I would have done anything,” Paulson said.
Paulson was one out of 20 patients enrolled in the clinical trial spearheaded by Seth Felder, MD, a colon and rectal surgical oncologist, and Jessica Frakes, MD, a radiation oncologist.
“Previously, in the context of rectal organ preservation or nonoperative management strategies, most rectal cancer trials have looked at trying to intensify chemotherapy, for example, using a stronger chemotherapy regimen on a patient in hopes that it may improve tumor response,” Felder said.
In this clinical trial, patients underwent a typical treatment process, including chemotherapy and radiation. Three weeks into radiation, the treatment changed depending on how each patient tolerated treatment and the change in volume of their specific tumor, indicating treatment response.
“What we did was at three weeks into the radiation, we took another set of images that our radiologists specifically reviewed, and they compared the volume of tumor at diagnosis to three weeks into radiation,” Frakes said. “We took the imaging at three weeks and used that to plan a radiation boost, specifically based on that patient’s tumor characteristics at that time.”
Using MRI technology, the personalized radiation was administered directly into the tumor itself.
“So far, we have had the majority of patients maintain a clinical complete response, and also, we are not seeing additional side effects that would give us pause,” Frakes said.
According to Felder and Frakes, when a patient appears to have had a complete response after receiving treatment, being checked frequently in surveillance is critical for recurrence, with this risk decreasing significantly two years post-treatment.
“There is a significant proportion of patients who have not had to have their rectum removed at this time, although we are awaiting longer term follow-up,” Felder said. “More than 15 out of the 20 patients have been able to avoid surgery fully.”
The 20th patient enrolled in the clinical trial is approaching the one-year mark post-treatment. As for Paulson, he just passed his two-year mark and remains cancer free.
“This didn’t prevent me from continuing to do what I love and living how I want,” Paulson said. “The compassionate care I received from Dr. Seth Felder, Dr. Sarah Hoffe and my entire care team at Moffitt made the whole journey so much easier to go through.”
Felder and Frakes hope this pilot study will lead to an even bigger multi-institutional study that can improve rectal cancer outcomes and treatment.