Experimental Drug Shows Promise for Patients With Rare Lung Cancer Mutation
An experimental oral drug called zoldonrasib has shown encouraging results for patients with non-small cell lung cancer carrying the rare KRAS G12D mutation. Results of a new multi-site study, including Moffitt Cancer Center, were presented at the American Association for Cancer Research Annual Meeting.
The drug is a first-of-its-kind treatment that targets the active form of the KRAS G12D mutation, offering hope for patients who currently have few options after standard treatments fail.
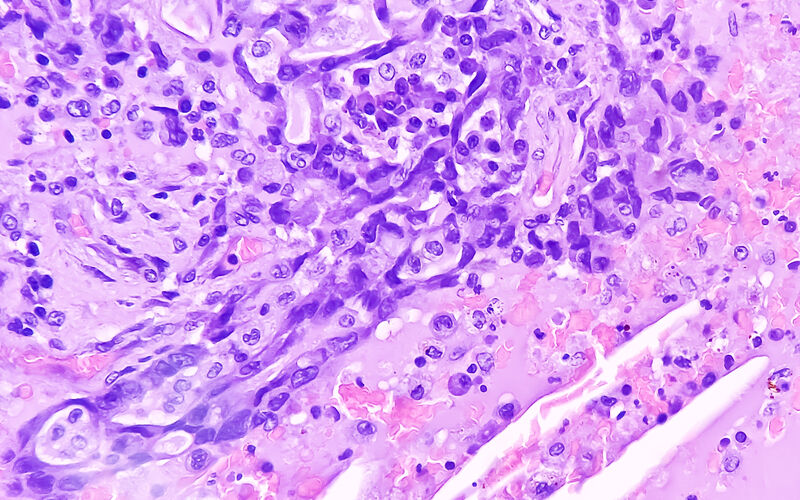
KRAS G12D mutations are a specific change in a gene called KRAS, which helps control how cells grow and divide. The KRAS gene normally makes a protein that acts like an on/off switch for cell growth. In healthy cells, KRAS switches on when growth is needed and off when it’s not. A mutation in KRAS can break this system.
The G12D mutation means that at position 12 of the KRAS protein, the normal amino acid glycine is replaced by aspartic acid.
About 4% of NSCLC cases involve the KRAS G12D mutation, and no approved targeted therapies exist for this group.

Eric Haura, MD
“Clinical trials such as this one with zoldonrasib are part of a larger strategy to identify best or first in class agents for patients with RAS gene mutations,” said Eric Haura, MD, associate center director for Clinical Science and director of the Lung Cancer Center of Excellence at Moffitt. “These results bring great hope to patients with KRAS mutations and their families.”
In an early phase clinical trial, researchers found that the drug was generally well tolerated, with no severe treatment-related side effects. The most common side effects were mild nausea, diarrhea, and fatigue.
Unlike existing KRAS G12C-targeted therapies, which lock the KRAS protein in an inactive state, zoldonrasib targets the active form of the protein. This approach may make it harder for tumors to develop resistance.
Among 18 patients with NSCLC who had been on the drug for at least eight weeks, 61% experienced a substantial reduction in tumor size, and 89% achieved disease control, meaning their cancer either shrank or stabilized.
These early results compared much better to standard chemotherapy treatments, which have a typical response rate of just 10% to 15% in this patient group. While the findings are promising, larger studies with longer follow-up are needed to fully understand the drug’s impact.
“While the results are very encouraging, we still need more research to understand why some patients with KRAS mutations do not have good responses to these agents as well as understand why tumors develop resistance,” said Haura. “We also need to develop new combination strategies with other agents to improve outcomes for patients with KRAS mutations.”