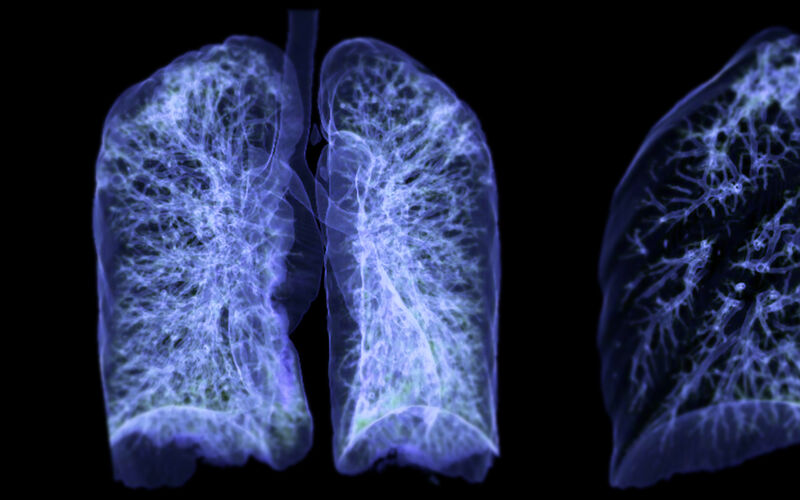
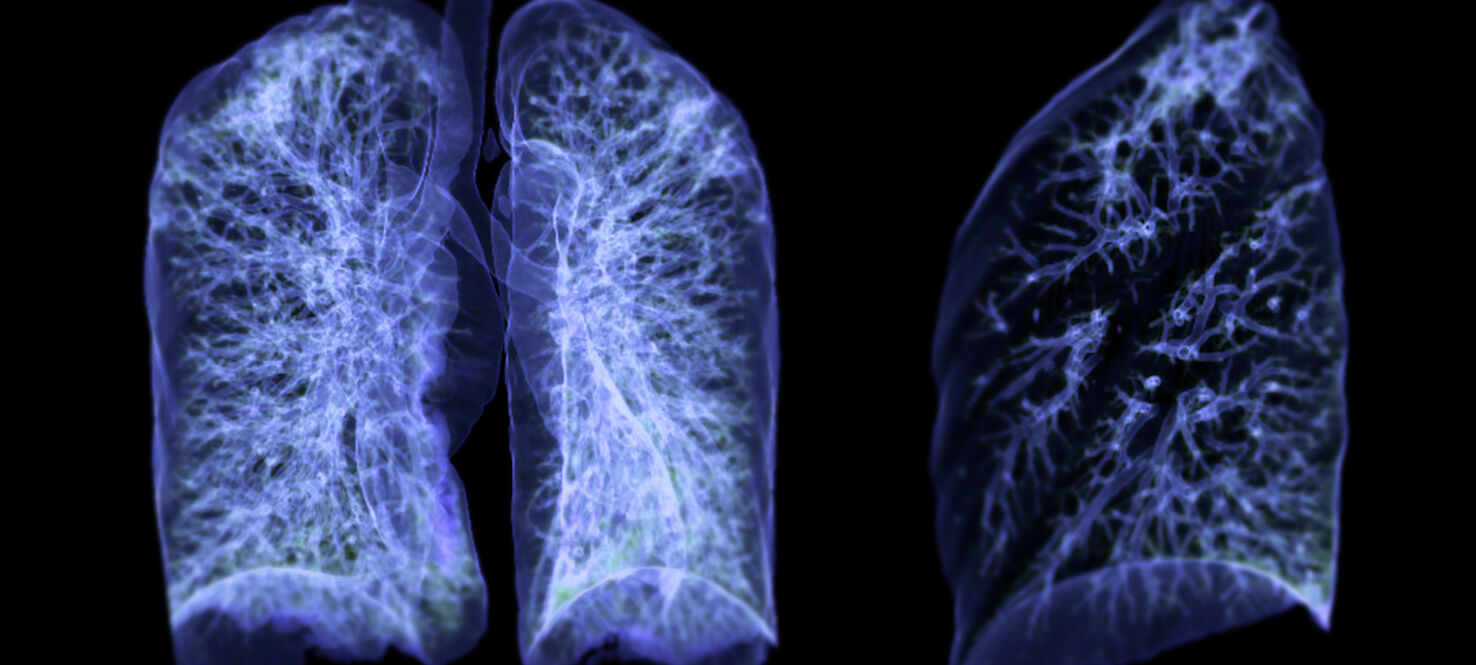
Flipping the Switch: New Moffitt Research Offers 2 Ways To Outsmart Drug Resistance in Lung Cancer
For years, researchers have been working to outmaneuver one of cancer’s most stubborn foes: KRAS, a gene that fuels tumor growth when it becomes stuck in the “on” position. New drugs that specifically target KRAS G12C mutations have given patients with certain types of lung cancer new hope, but the problem has been durability. Many tumors eventually find a way around these treatments.
According to the Lung Cancer Foundation of America, approximately 15–25% of patients with non-small cell lung cancer have a KRAS mutation, with the G12C subtype being the most common, found in about 10–14% of cases.
-
15–25%
Patients with non-small cell lung cancer that have a KRAS mutation
-
10-14%
G12C subtype is the most common
Now, two new studies led by researchers at Moffitt Cancer Center offer complementary ways to keep those tumors in check and even shut them down when they try to fight back.
Two Studies, One Goal: Stop Resistance Before it Starts
In one study, published in Cancer Research, researchers explored why some cancers stop responding to KRAS G12C drugs. They discovered that resistant tumors often reactivate the RAS signaling pathway, reigniting cell growth even in the presence of treatment.
Using next-generation compounds called RAS(ON) inhibitors, the team was able to block this reactivation and restore tumor control in preclinical models. These drugs work by targeting the “on” form of the RAS protein, essentially flipping the switch off again after cancer has found a way to turn it back on.
In a companion study also published in Cancer Research, the researchers looked at what happens inside cells that have already become resistant. They found that these cells develop a weakness and rely more heavily on proteins that help repair DNA and manage cell division. When researchers used drugs that block CDK12 and CDK13, the resistant cells became trapped during mitosis and eventually died.
Together, the findings suggest a one-two punch for overcoming drug resistance using RAS(ON) inhibitors to prevent resistance and CDK12/13 inhibitors to attack it when it appears.
Building a Smarter Strategy

Eric Haura, MD
“Resistance to KRAS G12C inhibitors remains one of the biggest challenges in lung cancer treatment,” said Eric Haura, MD, senior author of the studies and associate center director for Clinical Science and director of the Lung Cancer Center of Excellence at Moffitt. “These studies show us not just how tumors escape, but also how to outsmart them. By targeting both RAS signaling and CDK12/13, we can make treatment responses more durable.”
KRAS mutations are among the most common genetic drivers of non-small cell lung cancer, the most common form of the disease. Until recently these mutations were considered “undruggable,” but KRAS G12C inhibitors like sotorasib and adagrasib changed that. This new research takes the next step by showing how to extend the benefit of those treatments through combination and sequential strategies.
From the Lab to the Clinic
The studies used advanced genomic and molecular techniques to map out how cancer cells rewire themselves when exposed to KRAS G12C inhibitors. The results point to several new therapeutic options that are now being explored for clinical development.
“These discoveries give us a clearer path forward,” said Haura. “They reinforce Moffitt’s mission to translate basic research into better care for patients as quickly as possible.”