How AI Is Helping To Improve Diagnosing Bone Marrow Disorders
Artificial intelligence could help standardize the diagnostic process for myelodysplastic syndrome (MDS), a group of blood cancers that is difficult to identify.
MDS can look similar to two early stage conditions, idiopathic cytopenia of undetermined significance and clonal cytopenia of undetermined significance. These disorders cause low blood cell counts, but the cell changes are not advanced enough to meet the criteria for MDS. Distinguishing them from MDS can take time and requires highly trained specialists. This process can be subjective and prone to diagnostic challenges.

Palak Dave, PhD
Palak Dave, PhD, a postdoctoral research fellow at Moffitt Cancer Center, is part of the team that helped develop the AI system. She recently presented their findings at the annual American Society of Hematology annual meeting.
“The main motivation of this work is to standardize the diagnosis process while also improving the precision and efficiency,” she said.
Why Diagnosing MDS Is Challenging
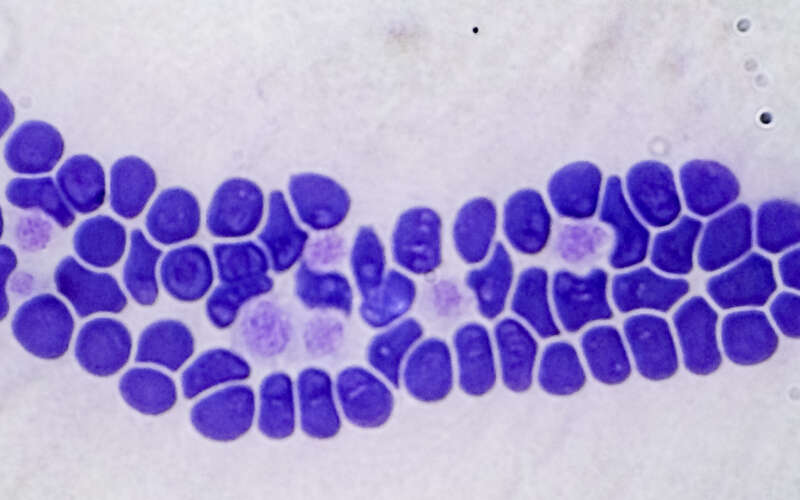
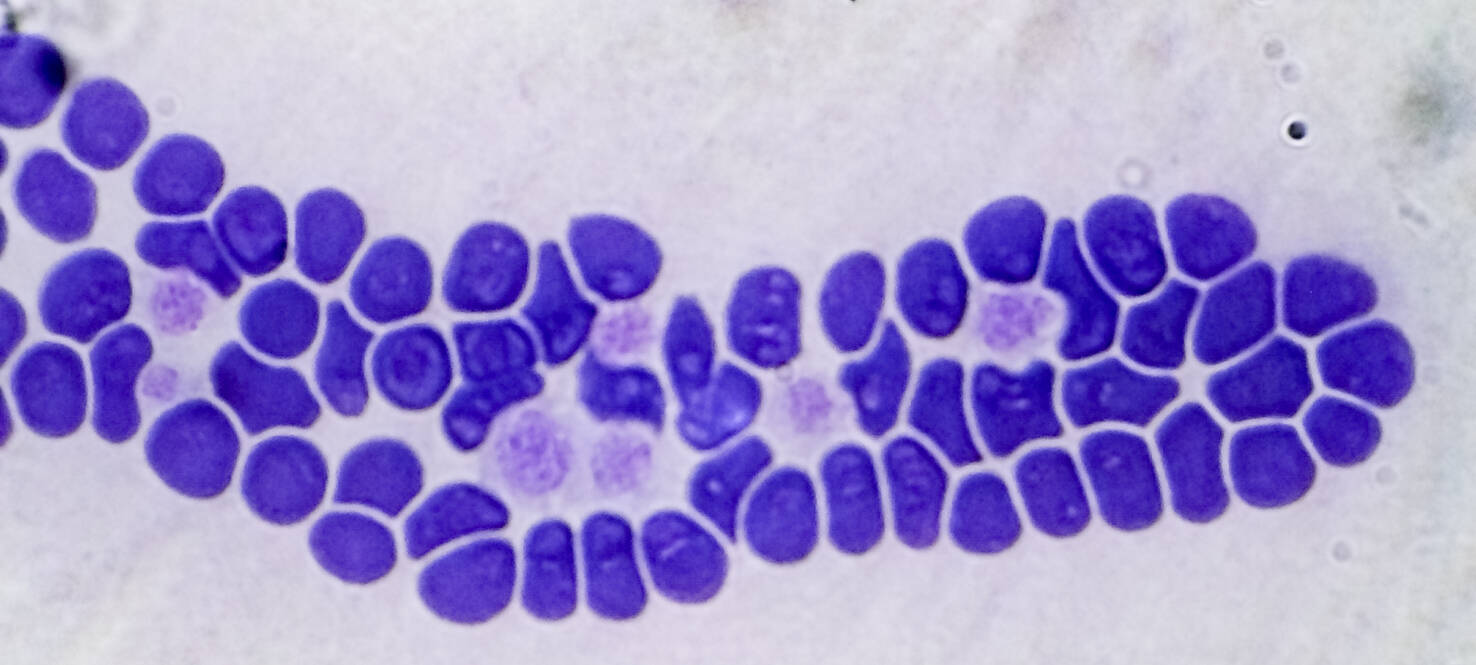
Current diagnosis depends on hematopathologists manually reviewing bone marrow slides. They look for specific abnormal features in individual cells and determine whether the abnormalities meet the threshold required to classify a case as MDS.
“It is kind of subjective,” Dave said. “There are a lot of subtle features that are involved in it. So, there can be a significant change in diagnosis from one person to another. There can also be significant changes in treatment decisions and the impacts down the line.”
Dave believes AI helps offer speed, efficiency, repeatability and reproducibility to the process. Another factor is access to testing. Some clinics rely on genetic information to support a diagnosis, but that is not always possible.
How AI Looks at Bone Marrow
The team built two models. One analyzed bone marrow aspirate smears. The other model examined bone marrow biopsy slides. Both samples are standard parts for diagnosing blood cancers. Aspirates show individual cells. Biopsies show the structure of marrow.
Processing time is quick at a minute or less per patient.
“We try to imitate what a human would look at as much as possible,” Dave explained. “The AI models are looking at the same samples at the same magnification level.”
The biopsy-based model was trained on 645 digitized slides from patients with either MDS or a pre-MDS condition. It was then tested on a separate group of 96 patients from another institution.
The biopsy model reached about 77% accuracy in the external test set. The aspirate model achieved about 85% accuracy in the same patients.
What’s Next?
Dave views this technology as promising but still developing.
“It is already doing a decent job and it has promise for the future,” she said. “If a human expert can verify what AI thinks is abnormal in a given sample, then that can be a big time saver.”
For this technology to be trusted, Dave notes explainability is essential. Her team is now working on that part of the project.
“These systems have to be able to explain their decisions,” she said. “We are trying to bring explainability into the system, so it is trustworthy from the physician or patient point of view.”
The group also plans to expand the AI approach to additional blood cancers.