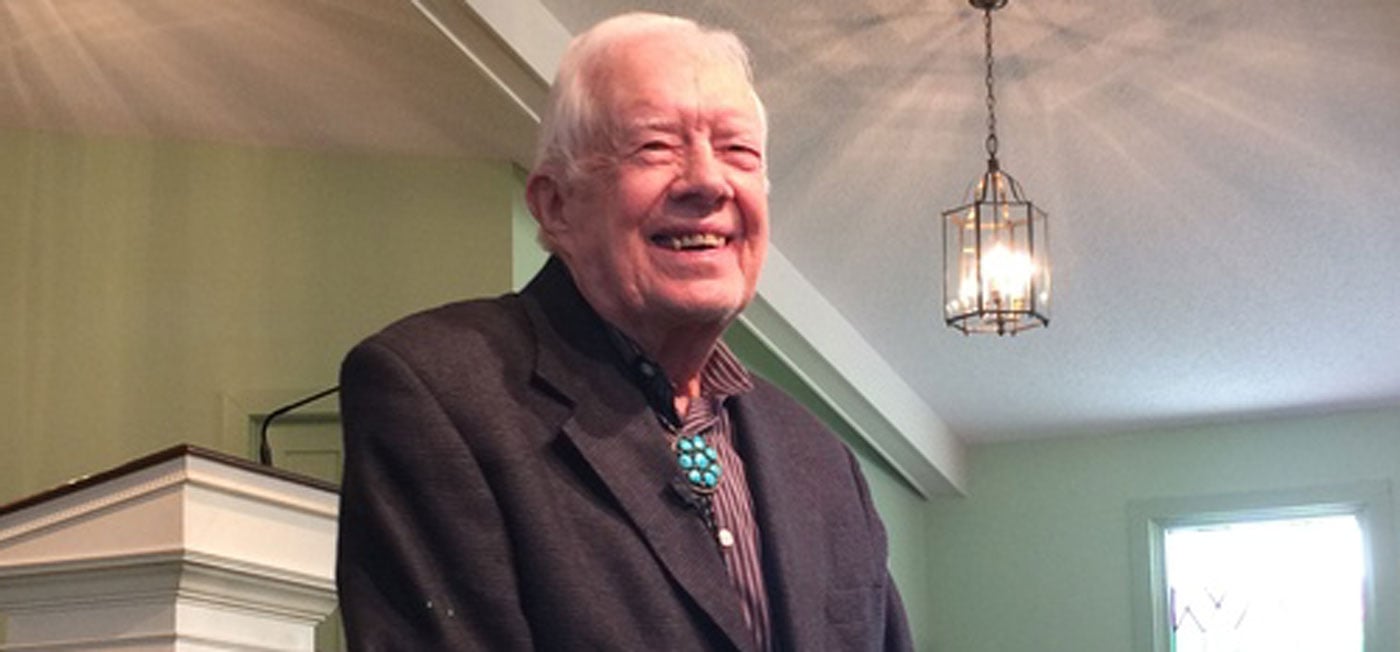
How Has President Jimmy Carter Survived Brain Cancer for 9 Years?
Former President Jimmy Carter’s melanoma metastasized to his brain in 2015. Nine years later, he is celebrating his 100th birthday.
It wouldn’t have been possible without immunotherapy — his doctors say the former president would not have lived much more than six months without it.
When the cancer spread to his brain, Carter was immediately considered a candidate for the checkpoint inhibitor ipilimumab, approved by the FDA just four years prior. Instead, his treatment team treated him with pembrolizumab, which the FDA authorized the year before.
Both treatments and other cancer immunotherapies are part of a new arsenal of treatments unavailable just a decade ago that are showing success in patients like Carter. This gives other patients with similar diagnoses hope, says Vernon Sondak, MD, chair of the Cutaneous Oncology Department at Moffitt Cancer Center.

“I frequently mention President Carter and his favorable experience when I discuss immunotherapy with patients,” Sondak said. “Especially older patients who are concerned about the side effects and impact on their quality of life.”
Alongside surgery, chemotherapy and radiation, immunotherapy is helpful in treating a range of cancers, not just melanoma. In Carter’s case, doctors also treated four tiny tumors in his brain with direct radiation treatments, and he had liver surgery.
“The advances in medical management of melanoma brain metastases are of great interest in general,” said Michael Vogelbaum, MD, PhD, chief of Neurosurgery and leader of the Neuro-Oncology Program at Moffitt. “Moffitt’s own Peter Forsyth, MD, chair of the Neuro-Oncology Department, accrued the highest number of patients for the study that helped prove that dual checkpoint inhibitor therapy (ipilimumab and nivolumab) is effective for melanoma brain metastases.”

Metastatic tumors like the ones that appeared in Carter’s brain are more common than primary brain tumors, which are cancers that originate and often stay entirely within the brain. Brain metastases occur when cancerous cells break away from the primary tumors — located in the skin in the case of most melanomas — and then travel to the brain via the bloodstream.
Approximately one-third of patients with cancer will develop brain metastases.
In 2021, Vogelbaum chaired an expert panel that led to the American Society of Clinical Oncology’s brain metastasis guidelines. The multidisciplinary panel of experts in neurosurgery, neurology, neuro-oncology, medical oncology and radiation oncology collaborated in a highly structured guideline development process. It is the first time that guidelines for brain metastasis included primary medical therapy as an option, as opposed to just surgery and/or radiation.
One of the main lessons that can be learned from Carter’s treatment is that age should not be a barrier to treatment with immunotherapies. Although older patients have weakened immune systems, doctors say the drugs can be effective in advanced age since the immune system remains active throughout life. However, older patients may be more likely to require breaks from the medication if they suffer side effects. Many patients develop skin rashes and flu-like fatigue from modern immunotherapy drugs, but some develop much more severe immune-mediated side effects, especially when combinations of drugs are used.