New Treatments for Breast Cancer Leptomeningeal Disease Using the Patients' Own Immune Cells
When cancer cells breach the protective barriers surrounding the brain and spinal cord, they create one of oncology’s most urgent clinical scenarios. Leptomeningeal disease (LMD) shifts what may have been a manageable cancer journey into a rapidly evolving neurological emergency where patients face declining function and traditionally limited therapeutic options.
LMD can progress from cancers such as lung cancer, melanoma, gastrointestinal cancers and hematologic malignancies. Breast cancer is especially likely to metastasize to the brain, with 10-15% of women with stage 4 breast cancer developing brain metastases. Once in the brain, it’s often deadly, with a typical survival outlook of two to three months.
Because LMD often emerges paradoxically when the systemic disease appears well-controlled, it creates a devastating disconnect between overall cancer response and neurological progression. Treatment options have historically been limited; however, scientific advances, such as those studied at Moffitt, are creating new opportunities for improved outcomes.
Leading the LMD Fight at Moffitt

Dr. Brian Czerniecki
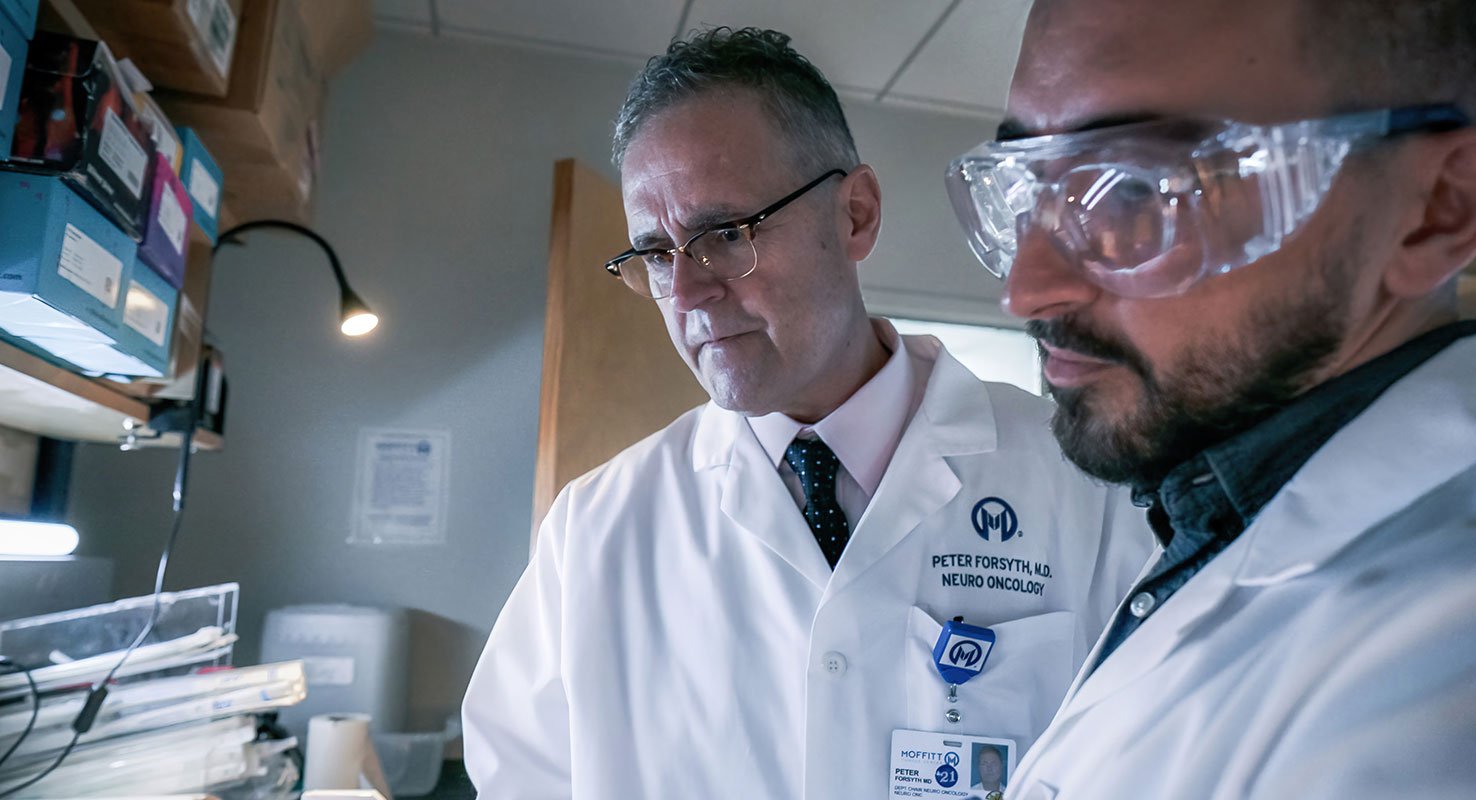
Under Dr. Peter Forsyth's leadership in the Neuro-Oncology Program, Dr. Brian Czerniecki's research into using immunotherapies and pioneering dendritic cell therapies for many years in the Breast Oncology Program, and Dr. Gary Koski's expertise in dendritic cell therapies at Kent State, they have secured significant Department of Defense recognition and funding to transform how we approach this complex disease from late-stage intervention to proactive and multidisciplinary management.
This initiative places Moffitt among a small cohort of institutions nationwide developing comprehensive strategies for earlier detection, improved specialized care coordination and accelerated research application for this devastating complication of breast cancer.
“This is an example of a special thing we do well at Moffitt, and that is to bring experts from many different fields together and focus like a laser beam on these unsolved cancer problems with the ultimate goal of curing and preventing them,” says Dr. Forsyth.
One current opportunity available to eligible breast cancer patients at Moffitt is a first-of-its-kind study investigating dendritic cell therapy (cDC1s) and its effectiveness in helping the body’s immune system better identify and attack cancer cells (MCC 21262). When the current treatment arsenal of established options is not enough, trials like this (NCT05809752) offer new hope.
This Department of Defense grant provides resources to study the biology of LMD in breast cancer, as well as two additional clinical trials to test these unique approaches to treatment for LMD. One of the clinical trials using dendritic cells will be opening in early 2026. The second clinical trial will open in late 2026.
“We just need to relentlessly push to understand the biology of this disease better all the time and get new therapies, available nowhere else in the world, available to our patients," says Dr. Forsyth. "We owe it to our patients to always have clinical trials and other treatment options available for them. I never want to say that I have no other treatment options to offer.”
Established LMD Treatment Options
Today's therapeutic landscape offers several approaches, each addressing different aspects of disease biology and patient needs.
- Intrathecal (IT) Chemotherapy: Delivered via lumbar puncture and used for hematologic malignancies or selected solid tumors.
- Systemic Therapy: Used for widespread disease or tumors known to cross the blood-CSF barrier. Targeted therapies have shown promising CNS penetration, and immunotherapy is currently being investigated.
- Radiation Therapy: Used to palliate symptoms caused by bulky leptomeningeal deposits. Whole-brain RT may be considered.
- Supportive and Palliative Care: Provides symptom relief for elevated intracranial pressure. Includes pain management, rehabilitation, and psychosocial support.
Breakthrough Emerging Therapies for LMD
Research initiatives currently underway are challenging historical outcome assumptions by leveraging emerging therapies.
Clinical Trials:
As part of the Neuro-Oncology Program’s expansion initiative led by Dr. Forsyth, Moffitt is enrolling patients in a clinical trial exploring the use of a dendritic cell vaccine administered intrathecally for HER2/HER3 patients with LMD from triple negative breast cancer or HER2+ breast cancer. A first-in-human dose escalation of a DCV administered intrathecally, this study’s purpose is to learn about the effects of this treatment and determine the highest dose that can be given safely to patients.
The dendritic cell vaccine is a cross between a vaccine and cell therapy administered into the fluid-filled space between the brain and the lining of the spinal cord. It is hypothesized to create a stronger immune response, empowering the body to identify and kill more tumor cells. This trial is only available at a few U.S. cancer centers, and Moffitt is proud to be one of them.

Dr. Kamran Ahm
Another open trial is studying the safety and effectiveness of radiation therapy followed by intrathecal trastuzumab and pertuzumab. Led by Moffitt’s Dr. Kamran Ahmed as the principal investigator, this trial explores whether the proposed treatment approach improves overall survival in HER2+ breast cancer that has metastasized to the leptomeninges.
Other trials are developing potential treatments using Tumor Infiltrating Lymphocytes (TILs), CAR-T therapies and drugs that target LMD metabolism.
Therapeutic Approaches:
Beyond investigational treatments, additional therapeutic advancements expand drug delivery options, utilizing nanoparticle-based therapies, convection-enhanced delivery and CSF liquid biopsies for real-time treatment monitoring.
The Power of Early Recognition
Successful outcomes depend heavily on recognizing disease development early on. Primary goals include identifying at-risk patients during early symptom phases, accelerating the evaluation processes, facilitating access to experimental protocols and targeted treatments, and coordinating comprehensive diagnostic workups for timely, accurate diagnosis.
Community healthcare providers should refer a patient with a cancer history to Moffitt for LMD evaluation and treatment when they develop new or worsening symptoms. These may include cranial nerve deficits, seizures, altered mental status (confusion, personality alterations, memory problems), unexplained headaches or nausea, radiculopathy and gait instability. Suspicious MRI findings are also cause for concern and warrant immediate referral for specialized evaluation.
Moffitt’s LMD Expansion
Moffitt’s LMD program expansion is transforming the treatment approach from crisis intervention to proactive, coordinated care. By eliminating traditional referral barriers and establishing dedicated pathways for prompt evaluation of patients at risk for CNS involvement, the program creates seamless access to LMD-specific expertise.
Moffitt's leading-edge research integrates with our specialized clinical care, ensuring patients can access the latest therapeutics while receiving the dedicated support and state-of-the-art resources that comprehensive cancer care demands.
To refer a patient to Moffitt, complete our online form or contact a physician liaison for assistance or support. As part of our efforts to shorten referral times as much as possible, online referrals are typically responded to within 24 - 48 hours.