Clinical Perspectives
Stay up-to-date with news and the latest in cancer care, created for and by healthcare professionals. MoffittBlogTM
275 Stories Found

Managing Common Non-Malignant Hematologic Disorders at Moffitt

Now Open: Moffitt at Speros Outpatient Center in Pasco County

Merlin Test Refines Melanoma SLNB Selection

The 2-3 Week Rule: When “Persistent” Symptoms Deserve a Cancer Evaluation
Direct Access to our Transplant and Cellular Immunotherapy Experts

The Critical Role of Surgeon Selection in Cancer Outcomes

Oncoplastic Surgery: Advancement in Breast Cancer Surgery

Expanding Access: Cellular Therapies and Autologous Stem Cell Transplants for Treatment-Resistant Autoimmune Disease

New Treatments for Breast Cancer Leptomeningeal Disease Using the Patients' Own Immune Cells
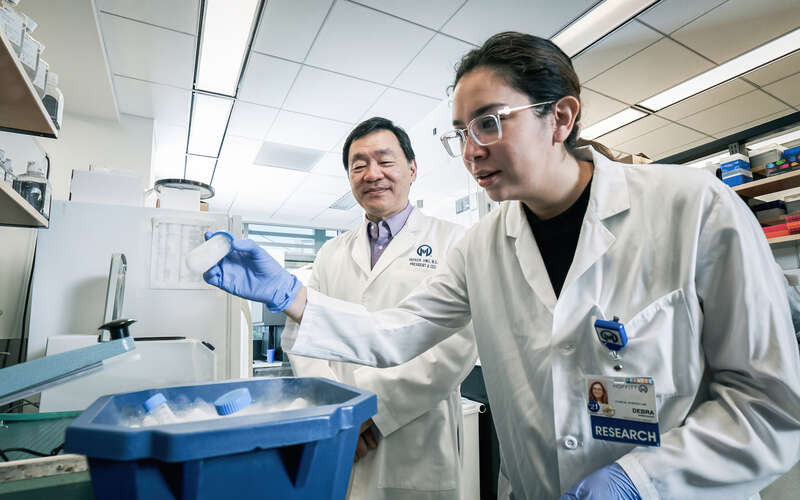
Personalized Breast Cancer Immunotherapy Trials

Expanding Treatment Horizons: Moffitt's Approach to Stage IV Esophageal Cancer Surgery

Improving Survival Rates in Esophageal Cancer: Why Early Referral Matters

Expanding Minimally Invasive Options for Lung Metastases: The Role of Thermal Ablation

6 Common Bone Marrow Transplant Misconceptions for Leukemia Patients

The Power of Investigator-Initiated Trials
