CAR T Breakthroughs and Patient Impact

Medically reviewed by John Cleveland, Ph.D., Executive Vice President, Center Director and Chief Scientific Officer at Moffitt Cancer Center
CAR T-cell therapy is often described as one of the most revolutionary breakthroughs in modern cancer care. By reprogramming a patient’s own immune cells to attack tumors, it has transformed once-fatal diagnoses into survivable conditions, inspiring hope worldwide. While many names are now associated with this therapy, its origins stretch back more than three decades to a small group of pioneering immunologists who reimagined what T cells could do to combat cancer.
Among them was Dr. Patrick Hwu, a young physician-scientist at the National Cancer Institute in the early 1990s, working alongside Dr. Steven Rosenberg and collaborating with Dr. Zelig Eshhar, who first conceptualized the chimeric antigen receptor (CAR). Together, this team laid the groundwork for what would become CAR T therapy. Dr. Hwu’s early experiments were among the first to show that human T cells could be genetically engineered to recognize and kill cancer, launching an entirely new field of medicine. Today, as President and CEO of Moffitt Cancer Center, Dr. Hwu continues to shape the future of cellular therapy, leading one of the country’s foremost centers for CAR T treatment and research.
CAR T-cell therapy, short for chimeric antigen receptor T-cell therapy, is a type of immunotherapy where a patient’s own T cells are engineered so they recognize and destroy cancer cells. T cells are collected from the patient, modified in the lab to express a synthetic CAR that targets a specific protein on tumor cells, expanded in number, and reinfused back into the patient. Once inside the body, these “supercharged” T cells bind to the target on cancer cells and eliminate them.
Unlike chemotherapy or radiation, which act broadly on all cells and tissues, CAR T works with precision by harnessing the immune system’s natural ability to fight disease and redirecting it to tumors it could not previously detect. The results in certain blood cancers have been remarkable. Patients with advanced leukemia or lymphoma who had limited treatment options have achieved complete, long-lasting remissions. The first FDA-approved CAR T therapy came in 2017, and today six CAR T products are approved for blood cancers, with thousands of patients treated worldwide.
The idea of a chimeric antigen receptor was first proposed in the late 1980s by Dr. Zelig Eshhar of the Weizmann Institute in Israel. He designed “T-bodies,” synthetic receptors that combined an antibody’s targeting ability with a T cell’s killing power. It was an ingenious concept, but it needed a clinical proving ground.
That proving ground was the Surgery Branch at the National Cancer Institute, led by Dr. Steven Rosenberg, a pioneer of adoptive T-cell therapy. In the early 1990s, Rosenberg’s team was already demonstrating that tumor-infiltrating lymphocytes (TILs) could be expanded and used to treat melanoma. Into this environment came Dr. Patrick Hwu, a physician with a passion for tumor immunology.
Working alongside Rosenberg and in collaboration with Eshhar, Dr. Hwu helped bring the CAR concept from idea to experiment. In 1993, he led a landmark study showing that human tumor-infiltrating lymphocytes could be stably modified with a CAR gene and redirected to specifically target and kill ovarian cancer cells. This was the first demonstration that CAR T technology could work in primary human immune cells against a solid tumor.
Two years later, in 1995, Dr. Hwu and colleagues published the first evidence that CAR T cells could function in living organisms. In mouse models of ovarian cancer, redirected CAR T cells prolonged survival, proving that this was not just a lab-based phenomenon. By the late 1990s and early 2000s, additional studies expanded on this foundation, but the initial breakthroughs had already been made. CAR T therapy was possible, and Dr. Hwu was one of the first to show it.
Dr. Patrick Hwu’s career has been inseparable from the rise of cancer immunotherapy. At the National Cancer Institute in the 1990s, he was part of Dr. Steven Rosenberg’s team that first proved tumor-infiltrating lymphocytes (TILs) could be expanded outside the body and reinfused to treat melanoma. He went further by engineering those T cells with chimeric receptors, demonstrating that it was possible to genetically reprogram immune cells to recognize tumors in a new way. These early experiments were a foundation not only for CAR T-cell therapy but also for modern cell therapy. Building on this work, Dr. Hwu later went on to lead the first phase 1 CAR T clinical trial in the United States for ovarian cancer patients.
Beyond his work on CAR T, Dr. Hwu also explored other strategies that have become central to immunotherapy. He investigated how cytokines such as interleukin-2 and GM-CSF could activate and sustain immune cells, and he conducted early clinical trials using gene-modified T cells in patients with ovarian cancer. This breadth of work positioned him at the crossroads of biology and translational medicine, helping bridge laboratory discoveries to patient care.
In 2003, Dr. Hwu was recruited to the University of Texas MD Anderson Cancer Center, where he built one of the country’s first departments dedicated to melanoma medical oncology and later led the entire Division of Cancer Medicine. Over 17 years there, he championed immunotherapies including checkpoint inhibitors, TIL therapy, cancer vaccines, and CAR T. He also mentored a generation of scientists and clinicians who would carry these therapies forward.
In 2020, he became President and CEO of Moffitt Cancer Center. In this role, he continues to shape the direction of cellular therapy research. Under his leadership, Moffitt has expanded its CAR T program, treating more than 2,000 patients to date, and is developing next-generation CAR T approaches aimed at solid tumors. Dr. Hwu’s unique combination of scientific insight and executive vision allows him to lead at both the bench and the bedside.
***In the American Society of Hematology’s (ASH) flagship publication, Blood, Dr. Steven Rosenberg and colleagues published one of the first reports showing that patients with advanced B-cell lymphomas could achieve objective tumor regression following CD19-directed CAR T-cell therapy, marking a milestone in adoptive cell transfer for hematologic cancers. The study demonstrated that genetically modified T cells could induce durable remissions in otherwise treatment-resistant lymphoma patients, establishing proof-of-concept for CAR T in the clinic.
By the 2010s, the concept that Dr. Hwu and his colleagues first tested in the early 1990s had become a reality. Patients with advanced blood cancers who were facing limited treatment options were achieving complete remissions with CAR T-cell therapy. The first FDA approval in 2017 marked a turning point in oncology and confirmed CAR T as a new standard of care.
At Moffitt Cancer Center, where Dr. Hwu now serves as President and CEO, CAR T has been embraced at scale. The center has treated more than 2,000 patients with CAR T-cell therapy for diseases such as lymphoma and multiple myeloma. The outcomes echo the early promise that Dr. Hwu saw decades ago. Many patients with otherwise lethal disease are experiencing durable, long-term responses in both clinical trials and real-world data.
Moffitt Cancer Center helped lead ZUMA-1, the first multicenter CAR T trial in adult lymphoma, co-led by Dr. Frederick Locke. Results from this study led to the FDA’s 2017 approval of Yescarta™ (axicabtagene ciloleucel). Soon after, Moffitt treated the first U.S. commercial patient with this groundbreaking therapy.
Dr. Hwu reflects on this milestone as deeply meaningful — what began as an experimental idea to redirect T cells has become a therapy that is saving lives.
First Approval - 2017: The FDA approves the first CAR T therapy based on decades of foundational work including Dr. Hwu’s early studies
2017–2024: Six CAR T products are approved in the United States for B cell leukemia, lB cell ymphoma, and multiple myeloma
Today and Beyond → Over 2,000 patients have been treated with CAR T at Moffitt Cancer Center, with many achieving durable responses

A powerful example of Moffitt’s leadership in CAR T is the story of Dimas, a non-Hodgkin lymphoma patient who entered Dr. Fred Locke’s clinical trial after running out of options — and today he is cancer free.
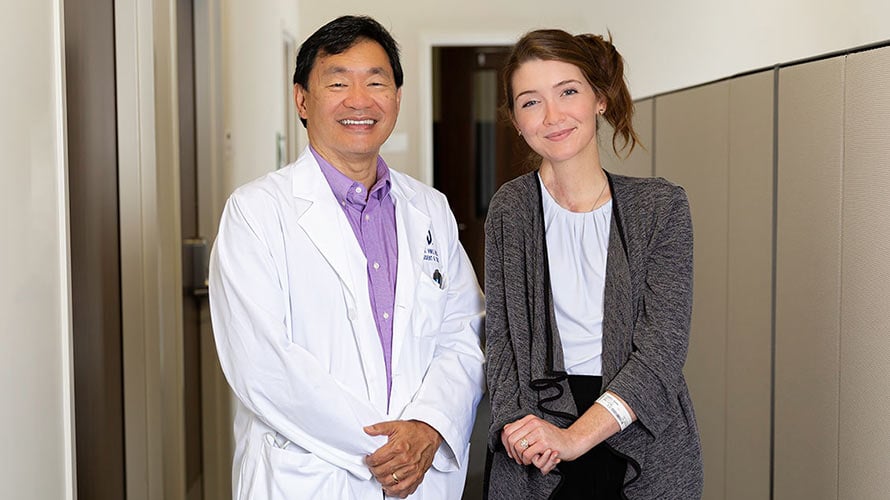
Dr. Patrick Hwu’s impact extends beyond the lab. He helped guide melanoma survivor Sara Leahey from patient to scientist, inspiring her to join his lab and later move with him to Moffitt Cancer Center in Tampa.
CAR T-cell therapy has transformed outcomes for many patients with blood cancers, but its full potential has yet to be realized. Solid tumors, which account for most cancer deaths, remain a significant challenge. This is where Dr. Patrick Hwu sees both opportunity and urgency.
As President and CEO of Moffitt Cancer Center, Dr. Hwu has made expanding the reach of CAR T a top priority.
This work builds on Moffitt’s experience treating more than 2,000 patients with existing CAR T therapies for lymphoma and myeloma, as of this writing, making it one of the country’s most active centers for cellular therapy.
Dr. Hwu’s decades of leadership in immunotherapy give him a unique perspective on how these advances can move from the lab into clinical reality. He often reflects on how remarkable it is to see CAR T move from an experimental idea to a therapy saving lives, and now to help shape its future so even more patients can benefit.
2,000+ patients treated with CAR T at Moffitt (as of this writing)
Clinical trials underway to expand into solid tumors
Research advancing CRISPR, dual-targeting CARs, and innovations to improve safety of CAR T therapies
Focus on off-the-shelf CAR T to improve speed and access
Researchers worldwide, including teams at Moffitt, are advancing new strategies to expand the impact of CAR T:
Expanding to solid tumors: Dual-targeting CARs, "switch" receptors, and CRISPR gene editing to make CAR T cells more resilient
Improving safety: Incorporating "suicide" switches and logic-gated CARs that reduce the risk of side effects such as cytokine release syndrome
Accelerating access: Allogeneic, off-the-shelf CAR T products are being developed to avoid manufacturing delays
Combining therapies: Pairing CAR T with TIL therapy, cancer vaccines, or oncolytic viruses to strengthen immune responses
The following frequently asked questions provide additional context on CAR T-cell therapy and Dr. Hwu’s contributions to its development.
CAR T-cell therapy, short for chimeric antigen receptor T-cell therapy, is a form of immunotherapy where a patient’s own T cells are collected, genetically modified to recognize cancer, and infused back into the patient to fight their disease.
The concept of CAR T was first introduced in the late 1980s by Dr. Zelig Eshhar. In the early 1990s, collaborations at the National Cancer Institute involving Dr. Steven Rosenberg and Dr. Patrick Hwu demonstrated that CAR-modified human T cells could target and kill cancer cells.
Dr. Hwu led some of the first studies proving CAR T cells could work in human immune cells and in living models. He also conducted one of the first CAR T clinical trials. These foundational experiments helped establish the scientific basis for CAR T therapy as it exists today.
Under Dr. Hwu’s leadership, Moffitt has treated more than 2,000 patients (as of this writing) with CAR T for B cell leukemia, lymphoma and multiple myeloma, and is running clinical trials to expand CAR T therapy into solid tumors. Moffitt is also investing in next-generation CAR designs and manufacturing innovations.
Researchers, including teams at Moffitt, are working to make CAR T therapies safer, faster, and more widely available. Advances include using CRISPR gene editing to create stronger T cells, developing off-the-shelf CAR T products, and designing receptors that can overcome the defenses of solid tumors.
CAR T therapy is available at select cancer centers, including Moffitt Cancer Center in Tampa, Florida, which offers both FDA-approved CAR T treatments and clinical trials testing new CAR T therapies.