HER2-Positive Breast Cancer Overview
HER2-positive breast cancer is a specific subtype characterized by the overexpression of the human epidermal growth factor receptor 2 (HER2) protein, which drives the rapid growth and division of tumor cells. This form of breast cancer accounts for approximately one in five cases and, while it is most commonly diagnosed in women, it can also affect men.
Significantly, HER2-positive breast cancer tends to develop and spread more quickly than other subtypes. On the other hand, it is also more responsive to targeted therapies designed to block HER2 signaling, an essential pathway that supports tumor growth. These advanced treatments can offer a more personalized and effective approach to HER2-positive breast cancer care, potentially improving the patient’s outcome and quality of life.
What causes HER2-positive breast cancer?
The underlying cause of HER2-positive breast cancer is not fully understood. Researchers believe it arises from acquired gene mutations that lead to an abnormal increase in HER2 protein production. Rather than being passed down through families, these changes occur during an individual’s lifetime.
Although the HER2 protein plays a positive role in healthy cell growth and repair, its overactivity in cancer cells can drive tumor development and progression. Understanding what contributes to its overexpression remains a key area of active scientific study.
What are the risk factors for HER2-positive breast cancer?
HER2-positive breast cancer can potentially affect anyone. However, certain factors may increase the risk. These include:
- Female gender – HER2-positive breast cancer predominantly affects women; diagnoses in men are rare.
- Genetics – A family history of breast cancer may increase an individual’s overall risk; however, HER2 status itself is not inherited.
- Hormonal factors – Early-onset menstruation, late-onset menopause and hormone replacement therapy may increase breast cancer risk in general.
- Radiation exposure – Prior radiation therapy delivered to the chest, particularly during adolescence or early adulthood, may slightly increase the risk of radiation-induced breast cancer.
- Unhealthy lifestyle – Obesity, excessive alcohol consumption and lack of physical activity may contribute to breast cancer risk, although these factors are not specific to HER2-positive cancer.
- Young age – While breast cancer risk increases with age, HER2-positive breast cancer is often diagnosed at a younger age than other subtypes.
Unlike many other forms of breast cancer, HER2-positive breast cancer is not strongly linked to inherited gene mutations, such as BRCA1 and BRCA2. Through ongoing research, scientists continue to explore how molecular and environmental factors may interact to influence HER2 status.

When diagnosed with breast cancer, Janelle found herself intimidated, but her niece Isabella gave her courage and inspired her to persevere and make a difference.
Request an AppointmentWhat are the symptoms of HER2-positive breast cancer?
The warning signs of HER2-positive breast cancer are generally similar to those of other subtypes. Early stages are often asymptomatic, with detection typically occurring through a routine screening test, such as a mammogram. As the tumor progresses, symptoms may become noticeable, such as:
- A new lump or thickening in the breast or underarm area
- Changes in the size, shape or appearance of the breast
- Unexplained breast pain or tenderness
- A newly inverted or retracted nipple
- Nipple discharge other than breast milk, especially if it is clear or bloody
- Redness, swelling or warmth in the breast
- Breast skin changes, such as dimpling, puckering or a pitted texture similar to an orange peel (peau d’orange)
Because HER2-positive breast cancer tends to grow and spread more quickly than other subtypes, its symptoms may develop and worsen at a faster rate. This underscores the importance of promptly discussing any unusual breast changes with a physician, as early detection offers the best chance for successful treatment.
How is HER2-positive breast cancer diagnosed?
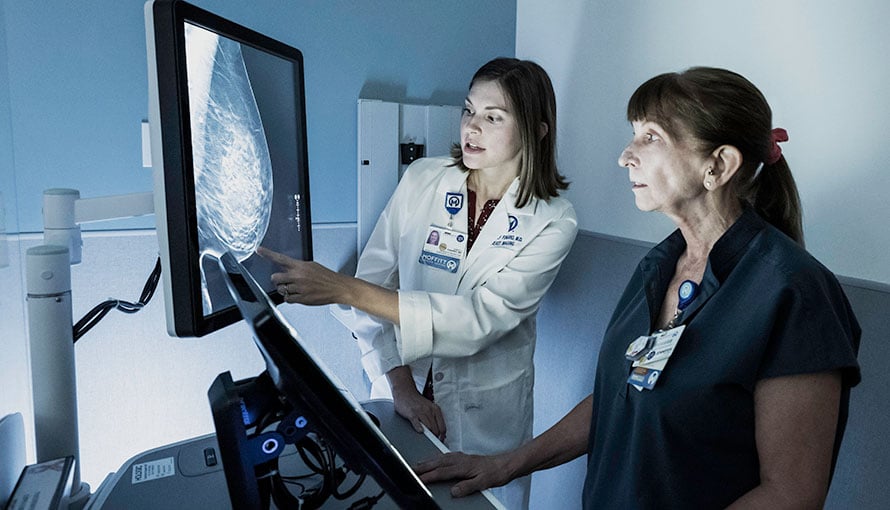
HER2-positive breast cancer is usually diagnosed through a multi-step process that includes a clinical breast exam, imaging studies, a biopsy and specialized lab work to determine HER2 status. Because HER2-positive tumors may respond well to targeted therapies, an accurate diagnosis is essential to guide treatment planning.
Typically, the diagnostic process for HER2-positive breast cancer includes:
Imaging tests
The initial evaluation typically begins with imaging studies to check for abnormalities in the breast tissue. Common breast imaging techniques include:
- Mammogram – A low-dose X-ray of the breast may reveal unusual masses, tiny calcium deposits (microcalcifications), architectural distortions or areas of dense tissue that may require additional imaging.
- Breast ultrasound – Often used to further assess abnormalities found on a mammogram, ultrasound can help the physician distinguish between fluid-filled cysts, which are usually benign, and solid masses that may indicate cancer.
- Breast magnetic resonance imaging – Breast MRI may be recommended for a patient with dense breasts or known risk factors. It can also be used to help the physician evaluate the full extent of the tumor before surgery.
Biopsy
If imaging suggests the presence of a tumor, the physician will likely order a biopsy to confirm the diagnosis. Common breast biopsy techniques include:
- Core needle biopsy – Guided by real-time imaging, the physician will use a hollow needle to remove several small samples of tissue from the suspicious area of the breast.
- Surgical biopsy – If the result of a core needle biopsy is inconclusive or additional samples are needed for evaluation, part or all of the suspicious tissue may be surgically removed.
The collected tissue will be sent to a laboratory, where a pathologist will examine it under a microscope for evidence of cancer.
HER2 testing
If the biopsy result confirms a diagnosis of breast cancer, immunohistochemistry (IHC) is usually performed to determine the HER2 status of the tumor. IHC employs antibodies and specialized staining techniques to measure the level of HER2 protein on the surface of the cancer cells. A pathologist will examine the stained tissue under a microscope and, based on the intensity and pattern of the staining, assign an IHC score ranging from 0 to 3+:
- 0 or 1+ – The tumor is HER2-negative and unlikely to respond to HER2-targeted therapies.
- 2+ – The result is borderline or equivocal, requiring further testing to confirm HER2 status. Usually, this will involve fluorescence in situ hybridization (FISH), a highly sensitive molecular test that can detect HER2 gene amplification.
- 3+ – The tumor is HER2-positive, showing strong HER2 protein overexpression and suggesting the patient may benefit from HER2-targeted treatment.
How is HER2-positive breast cancer treated?
HER2-positive breast cancer is generally managed with a personalized treatment plan based on the stage of the tumor and the patient’s overall health. Because this type of cancer tends to grow and spread quickly, treatment usually begins promptly after diagnosis.
Targeted therapy for HER2-positive breast cancer
In many cases, a key component of HER2-positive breast cancer treatment is targeted therapy, which is designed to block the activity of the HER2 protein and help slow or stop tumor growth. Options may include:
- Trastuzumab (Herceptin) – This widely used medication is often given alongside chemotherapy for heightened treatment effectiveness.
- Pertuzumab (Perjeta) – This targeted therapy may be used in combination with trastuzumab and chemotherapy, which can be particularly beneficial in advanced or metastatic cases.
- Ado-trastuzumab emtansine (Kadcyla) – This chemically linked (conjugated) drug combines the HER2-targeting antibody trastuzumab with a chemotherapy agent (DM1), allowing targeted delivery of the drug directly to HER2-expressing cancer cells.
- Neratinib and lapatinib – These oral targeted therapies may be prescribed in specific situations, such as extended treatment following initial therapy or in cases of metastatic HER2-positive breast cancer where continued HER2 inhibition is needed.
Targeted therapy for HER2-positive breast cancer can significantly improve the patient’s outcome by directly targeting HER2-positive cancer cells while sparing healthy cells.
Chemotherapy for HER2-positive breast cancer
Chemotherapy is often used in combination with targeted therapy, especially for early-stage and locally advanced HER2-positive breast cancer. Treatment may be given:
- Before surgery – Chemo can shrink a tumor and make it easier to remove, possibly making breast-conserving surgery possible.
- After surgery – Chemo can help eliminate any microscopic cancer cells that remain after surgery, reducing the risk of recurrence.
Breast Cancer Outcomes
The goal of any cancer treatment is to achieve the most favorable outcome while minimizing side effects and ensuring the best possible quality of life. On average, Moffitt's breast cancer treatment survival rates are 1.5 times the national average.
Surgery for HER2-positive breast cancer
Surgical treatment options for HER2-positive breast cancer may include:
- Lumpectomy – Known as breast-conserving surgery, this procedure involves removing the tumor along with a slim margin of surrounding healthy tissue, preserving most of the breast.
- Mastectomy – This more invasive procedure involves removing the entire breast, which may be considered based on the size and location of the tumor and the patient’s preferences.
Lymph node evaluation or removal may also be performed to help the physician determine if the cancer has spread.
Radiation therapy for HER2-positive breast cancer
Radiation therapy is often a key component of a comprehensive breast cancer treatment plan. In many cases, it is administered after the tumor is surgically removed to help eliminate any remaining microscopic cancer cells and reduce the risk of local and regional recurrence.
Depending on the extent and stage of the tumor, radiation may be directed to the remaining breast tissue, chest wall or nearby lymph node regions, such as the axillary, supraclavicular and internal mammary nodes. To maximize the therapeutic outcome, it is often used in combination with other treatments, such as chemotherapy, targeted therapy and hormone therapy.
Radiation therapy for HER2-positive breast cancer generally follows the same principles as it does for other subtypes, but there are a few considerations that may make it unique in terms of treatment timing, coordination and sensitivity to concurrent therapies. These include:
Coordination with targeted therapy
The most notable distinction lies in how radiation therapy is coordinated with HER2-targeted therapies, such as trastuzumab and pertuzumab. These drugs can be administered concurrently with radiation therapy, especially in a post-surgical setting. However, careful planning is required to avoid increased risk of cardiac toxicity, as both radiation therapy (especially when delivered to the left side of the chest) and HER2-targeted therapy can affect heart function. Cardiac monitoring is often recommended throughout treatment.
Tumor behavior
HER2-positive breast tumors tend to be more biologically aggressive than other types, which may influence the decision to use radiation therapy more proactively. For example, it may be used to treat regional lymph nodes or areas with a high risk of cancer recurrence, even after mastectomy, depending on the size of the tumor and any lymph node involvement.
Integration with other treatments
Radiation therapy is typically one component of a multimodal breast cancer treatment approach. When treating HER2-positive breast cancer, the timing and sequencing of the various therapies are particularly important due to the rapid tumor progression potential and the need to begin systemic therapy promptly.
Hormone therapy for HER2-positive breast cancer
If a breast tumor is both HER2-positive and hormone receptor-positive (HER2-positive and ER/PR-positive), hormone therapy may be incorporated into the treatment plan alongside HER2-targeted therapies. Hormone-blocking medications work by preventing breast cancer cells from responding to female hormones, which can fuel tumor growth.
Options may include:
- Tamoxifen – This antiestrogen drug can be used by both premenopausal and postmenopausal women to inhibit estrogen from binding to the hormone receptors on the cancer cells, effectively preventing estrogen from promoting tumor growth.
- Aromatase inhibitors (AIs) – Typically used after menopause, this class of drugs can reduce estrogen levels in the body by blocking the enzyme aromatase, which is responsible for converting androgens (male hormones) into estrogens (female hormones). By lowering estrogen levels, AIs can help slow or stop the growth of cancer cells that rely on estrogen for growth.
These specialized drugs can also help reduce the risk of cancer recurrence by limiting the influence of hormone signaling on tumor development. As such, they can be an important part of a long-term cancer management plan for a patient with a hormone-sensitive HER2-positive breast tumor.
Benefit from world-class care at Moffitt Cancer Center
As a National Cancer Institute-designated Comprehensive Cancer Center, Moffitt is dedicated to advancing the understanding of HER2-positive breast cancer through extensive research. Our highly acclaimed Don & Erika Wallace Comprehensive Breast Program offers comprehensive diagnostic, treatment and supportive care services in a single location. We also have a robust portfolio of clinical trials, providing our patients with unique opportunities to be among the first to benefit from promising new therapies that are not yet available elsewhere.
If you would like to learn more about HER2-positive breast cancer, you can request an appointment with a specialist at Moffitt by calling 1-888-663-3488 or submitting a new patient registration form online. We do not require referrals.
