Immunotherapy Treatment Options for Melanoma
As the name implies, immunotherapy is a treatment method that encourages a person’s own immune system to fight cancer. It can be used alone or in combination with other treatments, such as surgery and radiation therapy. A cancer specialist’s decision to include immunotherapy to treat melanoma depends on many factors, including the stage and type of the malignancy and the patient’s overall health condition.
Schedule an appointment to discuss your eligibility for treatment. Call us at 1-888-663-3488 or request an appointment online.
Different Types of Immunotherapy for Melanoma
There are two primary ways that different immunotherapies empower the body to combat cancer:
- Using drugs to stimulate the immune system’s natural defenses to identify and attack cancer cells
- Administering to melanoma patients substances that have been engineered to simulate cancer-fighting immune system components
The U.S. Food and Drug Administration (FDA) has approved the use of several types of immunotherapy as treatment for melanoma. Here’s a brief description of some of them:
Checkpoint inhibitors
This is a newer type of immunotherapy that has shown a lot of promise for patients with advanced stages of melanoma. "Checkpoints" are proteins on immune cells that must be switched off to allow an immune system response to become fully engaged. Sometimes, melanoma cells use checkpoints to evade the body’s immune system attacks. Immune checkpoint inhibitors are drugs that are designed to target and block these checkpoints, thereby allowing the immune system to effectively attack the melanoma cells.
For example, nivolumab, a prescription medication marketed under the brand name Opdivo, is an FDA-approved immunotherapy that’s often used to treat advanced melanoma that can’t be removed by surgery. It can also be used after melanoma surgery to reduce the risk of cancer regrowth, which is a treatment method known as adjuvant therapy.
How does it work? Opdivo blocks the activity of a checkpoint protein so that the body’s T cells recognize and attack melanoma cells. Studies have shown that combining Opdivo with another immunotherapy drug—ipilimumab, marketed as Yervoy—can extend the lifespan of patients with metastatic (advanced) melanoma.
Pembrolizumab (Keytruda) is another immune checkpoint inhibitor that is an FDA-approved treatment for melanoma. Like other immunotherapy medications, it is usually delivered through intravenous (IV) infusion in an outpatient setting. Checkpoint inhibitors differ in how frequently and for how long they are given.
Oncolytic virus therapy
Oncolytic viruses are viruses that have been engineered in a laboratory to preferentially infect cancer cells. They are usually injected directly into tumors on or close to the skin. In addition to destroying the melanoma cells at the injection site, oncolytic viruses can attract the immune system to the tumor site, leading it to target and attack melanoma cells at other locations besides the injection sites.
Cellular therapies
This approach uses immune cells taken from a patient’s own body and grown in the laboratory that are then reinfused into the patient to attack melanoma tumors that have grown despite the use of other forms of immunotherapy. This approach requires the patient to have good heart and lung function and is very labor intensive; therefore, only a few centers (including Moffitt) currently offer this approach.
Dr. Amod A. Sarnaik and colleagues found that the tumor-infiltrating lymphocyte (TIL) therapy, lifileucel, produced durable responses in patients with metastatic melanoma and in February 2024 lifileucel (Amtagvi) was FDA-approved for the treatment of adult patients with unresectable or metastatic melanoma previously treated with a PD-1 blocking antibody, and if BRAF V600 mutation positive, a BRAF inhibitor with or without a MEK inhibitor.
Understanding & Managing Immunotherapy Side Effects
The use of immunotherapy is associated with side effects different than those associated with traditional chemotherapy. Most side effects are a consequence of over-stimulation of the immune system, leading the immune system to attack normal, noncancerous cells in the body.
Common Side Effects to Watch For
Most patients experience mild to moderate symptoms. Identifying these early is the best way to manage them effectively:
- Skin Reactions: This is often the first sign, appearing as rashes, redness, or itchy patches.
- Gastrointestinal Issues: Diarrhea or abdominal pain may indicate inflammation of the colon (colitis).
- Respiratory Changes: A new cough or shortness of breath could signal inflammation of the lungs (pneumonitis).
- Liver Inflammation: This is often detected through routine blood tests rather than outward symptoms, though jaundice (yellowing of the eyes or skin) can occur.
Less Common Systemic Effects
In some cases, immunotherapy can affect specialized systems in the body:
- Endocrine System: It can impact the thyroid, pituitary, or adrenal glands. This may lead to conditions like hypothyroidism or Type 1 diabetes, often presenting as extreme fatigue or increased thirst.
- Neurologic System: Rare symptoms include muscle weakness, persistent headaches, or "brain fog" and confusion.
- Cardiovascular System: Though uncommon, inflammation of the heart muscle can cause chest pain, lightheadedness, or shortness of breath.
-
105,000
New melanomas will be diagnosed in the U.S. in 2025
-
8,500
People in the U.S. will die from melanoma this year
Duration and Recovery: What to Expect
Understanding the timeline of immunotherapy side effects can help reduce anxiety and ensure you receive the right care at the right time. Unlike chemotherapy, which usually causes side effects shortly after an infusion, immunotherapy side effects are less predictable; they can appear at any time—during active treatment or even months after your last dose.
Because these reactions are driven by your own immune system, the recovery process focuses on "resetting" that immune response. Here is what that typically looks like:
- Resolution: Most side effects are reversible and gradually fade once treatment is paused or completed and the immune system returns to its baseline.
- Medical Management: If symptoms persist or are severe, doctors often prescribe corticosteroids (like prednisone) to "quiet" the overactive immune response and protect healthy organs.
- Long-Term Effects: While many issues resolve, some conditions—particularly those affecting the endocrine system (such as Type 1 diabetes or thyroid issues)—may cause permanent changes that require lifelong hormone replacement therapy.
Common Questions About Melanoma Immunotherapy
Choosing the right treatment for melanoma is a major decision. To help you navigate your options, we’ve answered the most common questions about how immunotherapy works, what to expect during treatment, and how to manage side effects.
-
What is the difference between immunotherapy and chemotherapy for melanoma?
While both are used to treat melanoma, they work differently. Traditional chemotherapy directly attacks and kills fast-growing cancer cells, while immunotherapy empowers your body's immune system to recognize, target, and destroy melanoma cells. Because it works with your natural defenses, immunotherapy may offer a more durable, long-lasting response than chemotherapy.
-
How is immunotherapy for melanoma administered?
Most melanoma immunotherapies, such as immune checkpoint inhibitors (like Opdivo or Keytruda), are delivered through an intravenous (IV) infusion in an outpatient setting. Other types, like oncolytic virus therapy, may be injected directly into tumors on or near the skin. The frequency and duration of treatment depend on the specific drug and your individual treatment plan.
-
Can immunotherapy be used after melanoma surgery?
Yes. When immunotherapy is used after surgery to reduce the risk of recurrence, it is called adjuvant therapy. Drugs like Nivolumab (Opdivo) are FDA-approved for this purpose, helping to "mop up" any remaining microscopic cancer cells and providing an extra layer of protection against recurrence.
-
What are the most common side effects of melanoma immunotherapy?
Because immunotherapy "boosts" the immune system, side effects often stem from the immune system attacking healthy cells. Common side effects include fatigue, skin rashes, diarrhea and flu-like symptoms. While most side effects are manageable and temporary, some can be more serious, involving inflammation of the lungs, liver, or endocrine glands. Early detection is key, so you should always report new symptoms to your oncology team immediately.
-
How long does it take for immunotherapy to start working?
Compared to chemotherapy, immunotherapy often takes longer to show results on scans because the immune system needs time to build a response. In some cases, tumors may even appear to grow slightly before they shrink, a phenomenon known as pseudoprogression. Your care team will monitor you closely using blood work and imaging to track your progress.
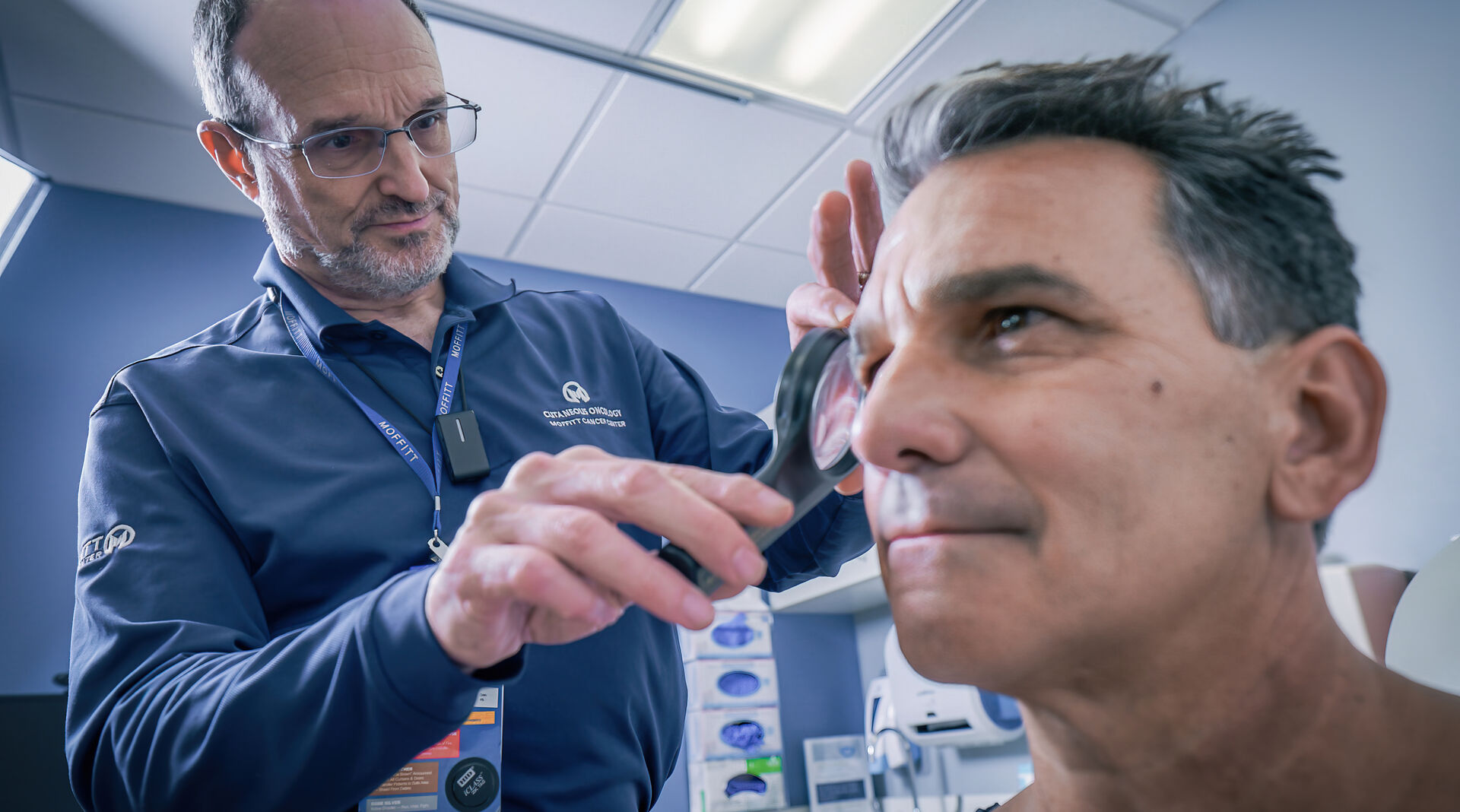
Moffitt's Approach to Treating Melanoma with Immunotherapy
The Cutaneous Oncology Program at Moffitt Cancer Center takes a multispecialty, patient-focused approach to the treatment of skin cancers. Our melanoma team comprises physicians from every treatment specialty—medical oncology, radiation oncology, surgical oncology, dermatology and others—all trained and experienced in the treatment of melanoma. Additionally, our cutaneous oncology team treats a high volume of cancer cases, including patients with complex and advanced-stage cancers. This translates into a wealth of melanoma treatment expertise that many other cancer hospitals can’t match.
Moffitt is a National Cancer Institute-designated Comprehensive Cancer Center, nationally renowned for its comprehensive treatment and supportive care, as well as its groundbreaking research and robust clinical trials program, which includes a wide range of immunotherapy options for melanoma and many other forms of cancer. As a result of our approach to melanoma treatment, our survival rates for patients with melanoma are significantly higher than the national average.
If you’d like to consult with an oncologist specializing in immunotherapy treatment options for melanoma, call 1-888-663-3488 or fill out a new patient registration form online. You don’t need a referral to visit Moffitt, and we’re committed to connecting every new patient with a cancer expert as soon as possible.
References
American Cancer Society – Immunotherapy
Melanoma Research Alliance – Opdivo (Nivolumab)
National Cancer Institute – Drugs Approved for Melanoma
AIM at Melanoma – FDA Approved Drugs
