A Mystery Rash, a Diagnosis Delayed
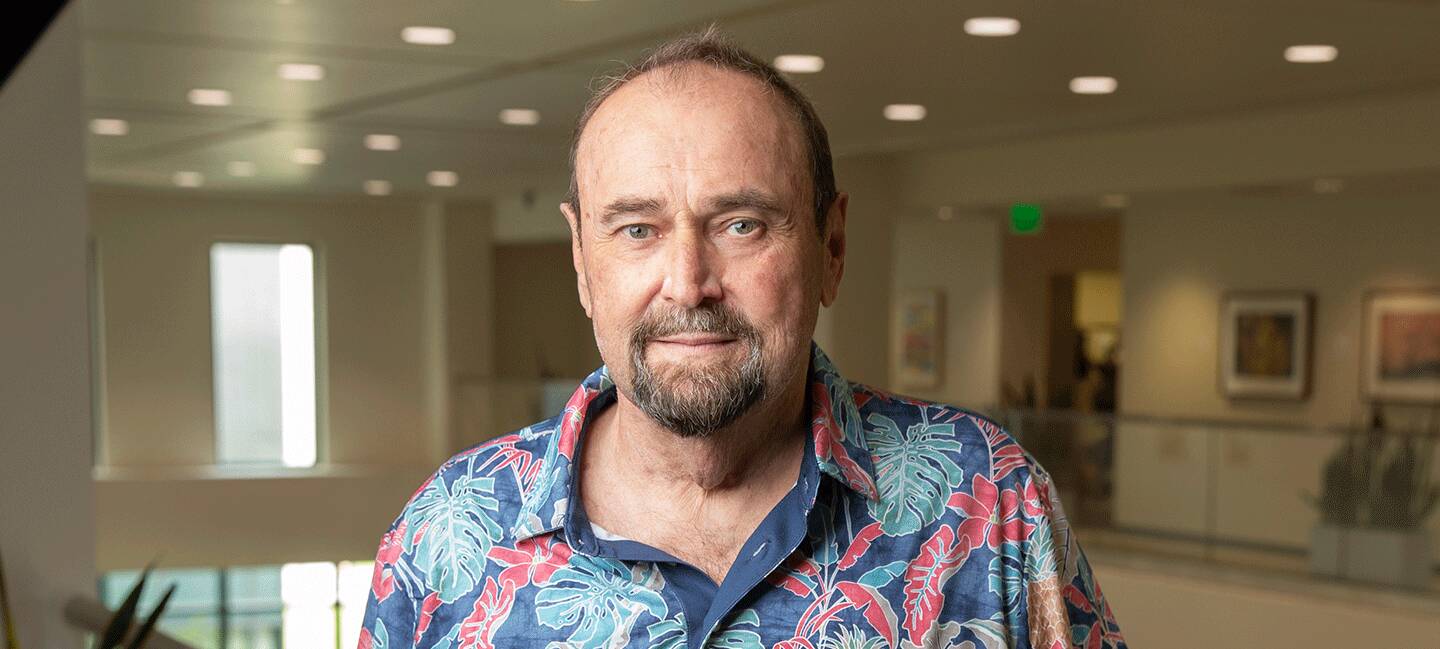
The trouble started in his hands. Larry Hart noticed his skin was peeling and cracking, sore to the touch. He had lost some sensation in his fingers and was having trouble doing simple tasks like opening a soda bottle.
This was around 2020 — the exact date didn’t stick in his mind. It didn’t seem like a major problem at the time.
His first stop was the dermatologist’s office. The doctor took a look and prescribed prednisone, a steroid used to treat common skin conditions like eczema and allergic reactions.

After years of searching for answers, Larry’s wife, Lynn, asked her dermatologist to look at a photo of her husband’s skin. The doctor told him to come in immediately for a biopsy.
For the next three years, Larry used prednisone off and on, along with other various hand creams.
“I tried a whole bunch of stuff,” he said. “Nothing would work.”
By the beginning of 2024, Larry was getting exasperated. The skin issues had been affecting both his hands and feet, and the medications weren’t helping. He decided to see an allergist, but first, he had to come off the prednisone.
“Exactly four days after I took my last prednisone, I began to look like I had the measles,” he said. “There were spots all over most of my body.”
That’s when the panic started to creep in.
Larry saw the allergist on Aug. 27, 2024, and was diagnosed with pityriasis rosea, another common skin condition that looks like a rash with oval spots. The allergist said it was caused by a viral infection and would go away on its own in a few weeks.
That was a Tuesday, just days before Labor Day. Larry and his wife, Lynn, were having the grandkids over for the holiday, and he had been looking forward to the visit at their Port Orange home. But the rash was getting worse, and the pain radiating from his skin was becoming unbearable.
On Sept. 2, he couldn’t take it anymore. He asked Lynn to take him to the hospital.
“It was breaking my heart that I missed my grandkids being here,” the 73-year-old said. “But it was pain that I can’t even describe. It was like taking the remote and changing the picture, holding your finger down and the picture keeps changing. Everything was flashing in my head. I couldn’t hold a thought, and I’ve never had anything like that in my life.”
At the emergency room, the medical team saw the bright red marks covering Larry’s body. But they, too, chalked it up to a viral skin infection. They diagnosed him with a panic attack instead. Larry again went home with no more clues into what was going on.
As Larry’s skin condition deteriorated over the next couple of weeks into what looked like open sores and welts, his wife had her own dermatologist appointment on Sept. 16 in Orlando. While she was there, she asked her dermatologist to look at photos she’d taken of Larry. The doctor told her: “Get him in here today.”
Lynn rushed Larry to her dermatologist, who performed a skin biopsy. One week later, and four years after his symptoms first began, they had a new diagnosis: cutaneous T-cell lymphoma.
“The doctor told me I had to immediately get an appointment with Moffitt,” he remembered.
A Rush for the Right Treatment
Cutaneous T-cell lymphoma (CTCL) is a rare type of non- Hodgkin lymphoma that originates in certain white blood cells and primarily affects the skin. In CTCL, white blood cells known as T lymphocytes begin growing uncontrollably, leading to what looks like a rash or ulcers on the skin.
About 3,000 people are diagnosed with the cancer each year in the United States, and many of them, like Larry, experience a long journey to answers. They are often misdiagnosed and treated for more common benign skin conditions like eczema. Meanwhile, the cancer progresses.
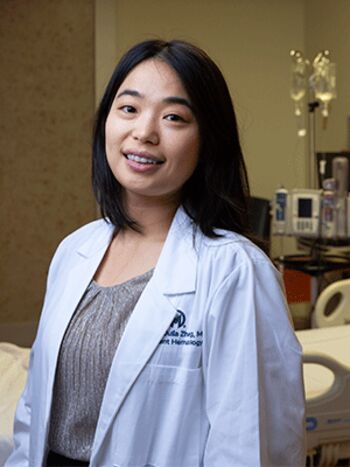
Yumeng Zhang, MD, who specializes in cutaneous T-cell lymphoma at Moffitt, is working to raise awareness about the rare disease.
Yumeng Zhang, MD, a hematology oncologist at Moffitt Cancer Center, specializes in cutaneous T-cell lymphoma. She initially saw Larry in October 2024 and immediately laid out a treatment plan to start total skin electron beam radiation therapy, a type of cutting-edge full-body radiation that is only available at a few medical centers in Florida. She quickly arranged with radiation oncologist Michael Montejo, MD, to schedule the first treatment.
For total skin electron beam radiation therapy, the patient typically stands with their hands above their heads, grasping a bar. However, in his condition, Larry couldn’t stand for very long, and he couldn’t make it through the first scheduled treatment.
When he returned to see Zhang on Nov. 14, 2024, she was torn. Larry needed that specialized radiation to treat his cancer, but his body as a whole was shutting down.
His skin was covered in painful tumors. He was in a wheelchair because he could no longer walk or stand for very long. His body had lost the ability to control its temperature, so he was shivering. His wife did most of the talking for him.
“I consider myself a pretty experienced doctor in cutaneous T-cell lymphoma, and at that moment, I was even scared,” Zhang said. “I could send him back to Dr. Montejo, and he could collapse, or I could send him to the hospital, but he wouldn’t get the most effective therapy for the disease.”
She made the tough call. Zhang worked with Montejo to squeeze Larry in for a total skin electron beam radiation session at Moffitt’s International Plaza clinic that afternoon. Montejo and his team made accommodations to provide the most comprehensive treatment possible, with Larry sitting for part of it. That evening, his wife drove him back to Moffitt’s Magnolia campus, where he was admitted for inpatient care.
Larry had finally started on the right treatment path, but the disease had ravaged his system. His body was going into renal failure from septic shock.
A Time of Touch and Go
Moffitt’s inpatient team rallied around Larry. They started him on dialysis, and he was transferred to the intensive care unit.
As he stabilized, Zhang worked closely with the inpatient care and radiation teams to get Larry started on chemotherapy and localized radiation treatment for the worst of the individual lesions.
“We were doing everything we could to control the disease,” Zhang remembered.
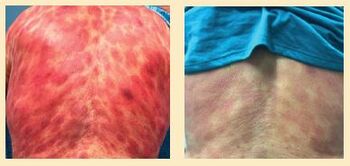
When Larry first came to Moffitt, his body was covered with painful lesions that had been misdiagnosed as common skin issues. With the right treatment, his cancer is now under control and the scars are fading.
Over the next 18 days in the hospital, Larry started to finally turn the corner. His body got stronger. The treatments began to shrink the tumors on his skin.
On Dec. 2, he transitioned to outpatient care. He completed eight sessions of total skin electron beam radiation therapy, finishing on Jan. 3, 2025. By the end of January, he was able to go off of dialysis.
By then, the bright red lesions on his back, chest, arms and legs had begun fading to a lighter shade of purple. His hands, the first sign of trouble, were back to normal.
Larry describes his recovery as “miraculous.” Zhang attributes it to the type of unparallelled multidisciplinary care that Moffitt provides.
“It takes a village to treat a patient, and this is the best example of it. We have medical oncologists, dermatologists, nephrologists, radiation oncologists, ICU doctors, our inpatient team and our advanced practice providers. All those specialties were able to work through things together,” she said. “If any one of us had fallen short, Larry wouldn’t be here today, and that’s what really makes a difference.”
Raising Awareness
For Zhang, Larry’s story is bittersweet. He has had a good outcome, but it shouldn’t have been such a long road to get there.
“We see this pattern too often — patients misdiagnosed. Then they get delayed treatment, and they deteriorate because this is a rare and easily mistaken skin disorder,” she explained. “That’s what’s scary, to hear his story, is that everything that he’s been through — it all started with a rash a few years ago that could be recognized. CTCL shouldn’t land patients in the ICU.”
When diagnosed early, patients may have the option of being treated with phototherapy, a type of ultraviolet light treatment, or other therapeutics that are more gentle on the body. Unfortunately, many of the patients who come to Zhang have been struggling to get an accurate diagnosis for years. One study, published in Dermatology and Therapy, surveyed more than 10,000 dermatologists and found that 91% reported that they tested for CTCL only after patients didn’t respond to treatments for more common skin conditions.

“The truth of the matter is that CTCL is extremely rare, so the awareness is low,” Zhang explained, “and that’s the job for me as an oncologist to do this.”
Zhang partners with Moffitt’s physician liaison team to connect with dermatologists and community physicians across Florida to spread awareness of CTCL, the symptoms, what is required for diagnosis and treatment options. She also works closely with community oncologists who continue treating her patients when they cannot make the regular drive to Moffitt. She does one-on-one calls, virtual consults and gives out her cellphone number.
Every patient she sees is motivation for her to do more.
“For every missed disease, you see a person behind it, you see a family and you see them looking for answers,” she explained. “That’s what resonates with me and what drives me.”
‘All This Could Have Been Averted’
With his cancer under control, Larry now sees a local oncologist near his home on the east coast of Florida for regular bloodwork and a bimonthly injection called Pegasus to prevent recurrence. He also sees a local dermatologist for phototherapy. Zhang works closely with his local care team to coordinate Larry’s ongoing treatment, and he returns to Moffitt every three or four months to see her. Although CTCL is incurable, Larry’s care team is working to prevent the chance of relapse.
After five long years of symptoms and a harrowing start to treatment, Larry is hopeful but hesitant.
“I’m starting to believe in my head that if I pinch myself, I’m going to wake up from a dream because I am absolutely feeling 100%. I don’t have any issues,” he marveled. “But this thing was prolonged for years. All this could have been averted if I was diagnosed a little sooner by people who were looking at me regularly. This didn’t need to get as bad as it did.”
This article originally appeared in Moffitt's Momentum magazine.
ON THE CUTTING EDGE OF CTCL CARE
Each year, more than 250 new patients are evaluated for cutaneous T-cell lymphoma through the renowned Multidisciplinary Cutaneous Lymphoma Clinic, a partnership between Moffitt Cancer Center and the USF Health Department of Dermatology. Spearheaded by Moffitt hematologist and oncologist Lubomir Sokol, MD, PhD, and USF Health dermatologist Lewis Frank Glass, MD, their clinic teams have assessed thousands of CTCL patients since its inception in 2004. Today, the clinic manages the care of more than 1,000 active patients, making it the largest CTCL referral hub in the Southeast.
This highly specialized, coordinated approach is critical to both the timely diagnosis and personalized treatment of such a rare and complex disease, Sokol emphasizes.
“Cutaneous T-cell lymphoma can mimic a wide range of common benign dermatologic conditions, making an accurate diagnosis exceptionally challenging and frequently delayed for years,” he explained. “Having a multidisciplinary team is not just helpful but it’s essential for the effective management of rare malignancies involving skin, blood and lymph nodes.”
Beyond diagnosis and care, Moffitt is at the forefront of innovation, working to expand CTCL treatment options through cutting-edge clinical trials. The cancer center currently leads two investigator-initiated studies, and plans are underway to launch a groundbreaking, multi-institutional trial aimed at accelerating CTCL research on a national scale.
“Progress in rare diseases like CTCL is often hindered by the small patient population,” Sokol noted. “That’s why collaboration across global centers is vital to designing and executing the large randomized studies needed to bring new therapies to patients faster.”