
Comparing TILs, CAR-T, and BiTEs: Advances in Immunotherapy for Targeted Cancer Treatment
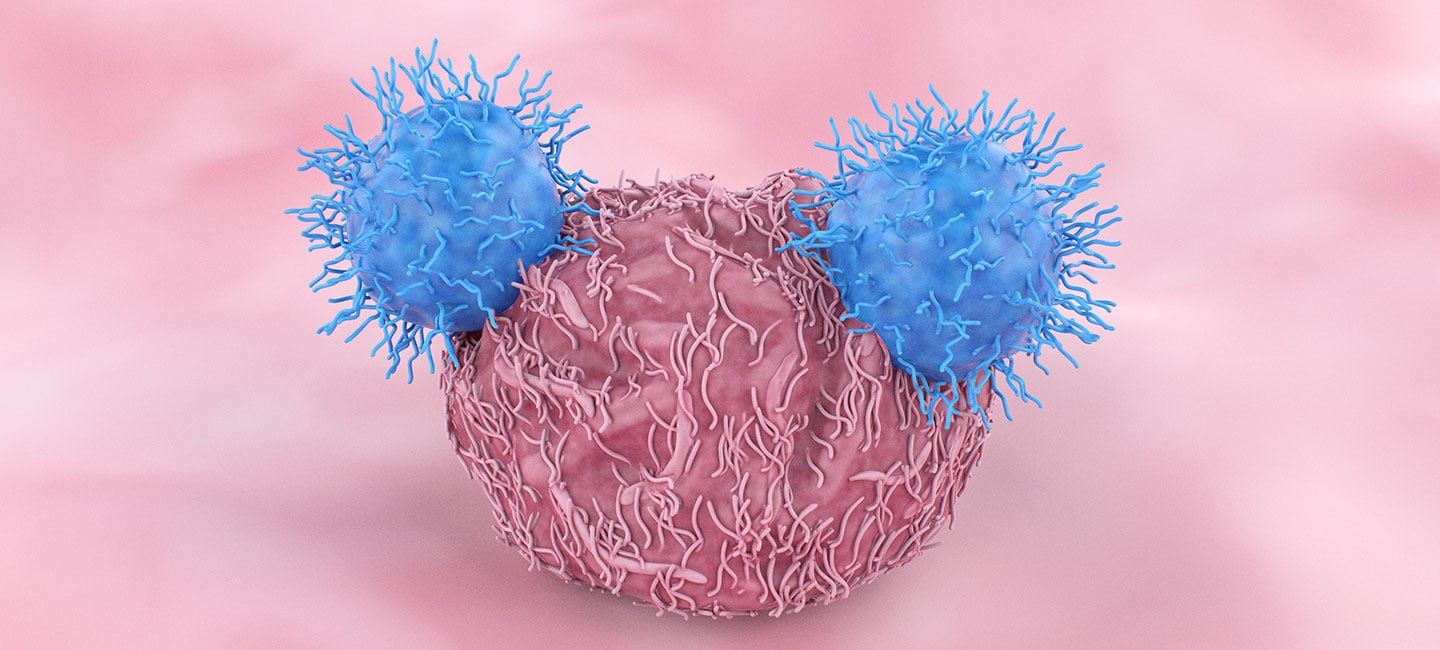
Over the last decade, cellular immunotherapy has revolutionized the treatment of many types of cancer. By harnessing the inherent strength of the body’s own defense mechanisms, these powerful tumor-fighting therapies build on the natural capabilities of the immune system, helping it to identify, attack and destroy cancerous cells.
As a globally recognized pioneer of novel cancer treatments, Moffitt Cancer Center is firmly positioned at the forefront of cancer research, particularly in the emerging field of immunotherapy. Through landmark clinical trials, our patients have unique opportunities to benefit from promising new therapies before those options are made available in other settings. Working closely with other respected cancer centers nationwide, we continue to make significant progress in advancing cancer treatment, creating a new source of hope for many current and future patients.
Physicians who are looking for advanced immunotherapy options for their patients should consider Moffitt and our commitment to groundbreaking research, clinical excellence and individualized care. The following outlines key similarities and distinctions between TILs, CAR-T, and BiTEs, providing insights for those looking to deepen their understanding of these immunotherapies and their applications in cancer treatment.
Tumor-infiltrating lymphocyte (TIL) therapy
TIL therapy is an advanced immunotherapy approach that capitalizes on the unique power of cancer-fighting lymphocytes that have already identified cancerous cells within the body, launched an attack and successfully invaded a tumor. After one cancerous tumor (primary or secondary) is surgically removed, the tissue is sent to a specialized laboratory for processing. There, the TILs within it are isolated from other tumor cells, cultured and multiplied with interleukin-2 (IL-2). A large quantity of TILs are then reinfused to the patient.
By leveraging the patient’s own immune cells that have naturally infiltrated a tumor and enhancing their potency through ex vivo expansion, this personalized therapy has shown great promise in treating metastatic melanoma. Additionally, scientists are currently evaluating the effectiveness of TIL therapy for other solid tumors, including:
Research and clinical trials conducted at Moffitt and other leading institutions have demonstrated significant tumor regression and, in some cases, durable complete responses, making TIL therapy a promising option for patients with relapsed or refractory tumors.
The multispecialty team at Moffitt has extensive experience in administering TIL therapy for melanoma and other solid tumors, and we consistently achieve outcomes that exceed national averages. Our patients benefit from comprehensive and individualized care, including pre-treatment evaluation, post-treatment monitoring and supportive care to manage any side effects as well as the myriad physical, mental and emotional challenges that often go along with cancer. Our renowned program is led by pioneering oncologists who have been and continue to be directly involved in developing and refining this innovative therapy, which is changing the lives of many patients.
2,000+ CAR T Patients Treated and Counting
Refer a PatientChimeric antigen receptor (CAR)-T cell therapy
A groundbreaking form of immunotherapy, CAR-T cell therapy involves genetically modifying a patient’s own immune cells. Through leukapheresis, white blood cells are collected from the patient’s blood. The isolated T cells are then sent to a specialized laboratory where the cells are genetically engineered to express a CAR that targets antigens specific to the patient’s cancer, bolstering the ability of the T cells to identify, attack and destroy tumor cells. The CAR-T cells are then reinfused to the patient.
In extensive research studies performed to date, CAR-T cell therapy has shown great promise in treating certain hematologic cancers, including:
- Relapsed and refractory acute lymphoblastic leukemia in pediatric and young adult patients
- Relapsed and refractory diffuse large B cell lymphoma in adults
- Relapsed and refractory follicular lymphoma
- Relapsed and refractory mantle cell lymphoma
- Multiple myeloma
- Primary mediastinal B cell lymphoma
Significantly, in certain cases where the tumor has not responded to other treatments, CAR-T cell therapy has led to considerable remission rates.
That said, CAR-T cell therapy is a highly complex, specialized and personalized cancer treatment. Additionally, managing its unique and potentially dangerous side effects—such as cytokine release syndrome—requires extensive training and practice. Therefore, to ensure the best possible outcome and quality of life, it is essential to entrust the care of your patients to an experienced multispecialty team at a high-volume, state-of-the-art cancer center. Moffitt has embraced the mission and responded with excellence.
As a world-renowned trailblazer in cancer research, Moffitt is spearheading the development of CAR-T cell therapy clinical trials in collaboration with other cancer centers across the nation. One notable example is Yescarta (axicabtagene ciloleucel), the first treatment of its kind to be approved by the U.S. Food and Drug Administration (FDA) for treating adults with certain types of non-Hodgkin lymphoma. Moffitt is proud to have made Yescarta available to the first patient in the world. We were also the first cancer center to treat more than 1,000 patients with CAR-T cell therapy.
Bispecific antibody treatment
A common type of targeted therapy for cancer, monoclonal antibodies are engineered in a laboratory to recognize a specific antigen found on the surface of tumor cells. The goal is to help the immune system target, attack and destroy cancerous cells. Widely considered to be the next generation of monoclonal antibodies, bispecific antibodies (BsAbs) take this treatment approach one step further. Engineered to simultaneously bind to two different antigens —one on a tumor cell and one on an immune cell—these drugs can bring cancer-fighting immune cells into close proximity with tumor cells, further enhancing the ability of the immune system to fight cancer.
A recent surge in new BsAbs—including a specialized subtype known as bispecific T-cell engagers (BiTEs)—is ushering in a new era in cancer treatment. Bispecific antibodies such as Blincyto (blinatumomab) have shown significant efficacy in treating acute lymphoblastic leukemia by targeting CD19 on B cells and CD3 on T cells, offering a novel and effective approach to cancer immunotherapy.
The scientists and clinicians at Moffitt have extensive experience with BsAbs and BiTEs, and our team is actively involved in research and clinical trials with the goal to expand their use to other types of cancer, such as:
- Non-Hodgkin lymphoma (NHL) – BsAbs can target specific markers on B cells in various subtypes of NHL.
- Multiple myeloma – BsAbs can target B cell maturation antigen (BCMA) on myeloma cells and CD3 on T cells.
- Certain solid tumors – BsAbs show promise in treating lung cancer, colorectal cancer and ovarian cancer.
Moffitt’s comprehensive care model integrates BsAbs with other therapeutic modalities, providing a holistic approach to cancer treatment that addresses all aspects of the patient’s health and well-being.
Refer a patient to Moffitt Cancer Center for cutting-edge immunotherapy treatment
When you refer a patient to Moffitt for TIL therapy, CAR-T cell therapy or BiTEs treatment, you can feel confident that they will receive attentive care from a multispecialty team that includes some of the foremost experts in the world. You can also expect to receive timely and informative updates from us on your patient’s progress. It is our privilege to collaborate with referring physicians. Working together, we can improve outcomes and quality of life for our shared patients.
Moffitt has implemented an effective cross-departmental program to bring pivotal immune cell therapies to our patients quickly and safely. As principal investigators, disease-specific experts maintain oversight of these key studies, while clinical care and trial coordination are centralized to leverage the expertise and infrastructure of our already robust clinical trials program.
If you would like to refer a patient to Moffitt for immunotherapy, complete our online form or contact a physician liaison for assistance or support.
