Breast Cancer Surgery: Dispelling the Myths
For many people with breast cancer, surgery is a cornerstone of treatment, often alongside radiation therapy or chemotherapy. Studies consistently show that surgical procedures such as lumpectomy and mastectomy are highly effective in removing breast tumors, reducing the risk of cancer recurrence and helping the patient achieve the best possible outcome and quality of life.
Even so, misconceptions about breast cancer surgery abound, often causing unnecessary fear, anxiety, and confusion during what is already an emotionally charged time. Misinformation may lead some individuals to delay treatment, misunderstand their options or have unrealistic expectations about the outcome. At Moffitt Cancer Center, we prioritize patient education and support. We know that when a patient has all the facts about breast cancer surgery, they can make the best possible decisions about their care and approach their procedure with greater confidence.
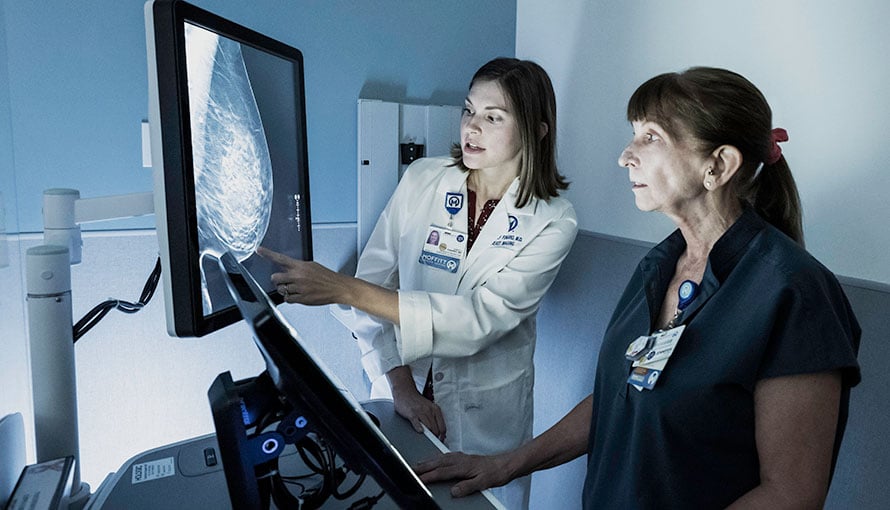
Toward that end, the multispecialty team in Moffitt’s nationally acclaimed Don & Erika Wallace Comprehensive Breast Program can debunk several common misconceptions about breast cancer surgery:
Misconception #1: Mastectomy is always more effective than lumpectomy plus radiation therapy.
For most early-stage breast tumors, surgery is the preferred treatment method. Many patients have a choice between two procedures: lumpectomy (breast-conserving surgery) or mastectomy. Lumpectomy involves removing only the tumor and a slim margin of surrounding healthy tissue, preserving most of the breast, while mastectomy involves removing the entire affected breast.
Some patients may lean toward mastectomy over lumpectomy based on the assumption that removing the entire breast is always more effective in eliminating cancer. However, the evidence does not support this belief. Extensive research on patients with early-stage breast cancer has shown that survival rates are nearly identical between those who undergo lumpectomy followed by radiation therapy and those who opt for mastectomy. These findings highlight that both approaches can be equally effective, depending on the individual case.
The decision between breast-conserving surgery and mastectomy is deeply personal. A patient should make this choice only after carefully weighing the benefits and risks of each approach. It is important to remember that, for most individuals with early-stage breast cancer, survival outcomes are comparable regardless of the surgical option selected.
Breast Cancer Outcomes
The goal of any cancer treatment is to achieve the most favorable outcome while minimizing side effects and ensuring the best possible quality of life. On average, Moffitt's breast cancer treatment survival rates are 1.5 times the national average.
Misconception #2: Breast surgery causes cancer to spread.
After undergoing a lumpectomy or mastectomy, some patients are later diagnosed with a tumor in another part of their body. This has led to a common misconception that cancer cells are released into the air during breast cancer surgery, allowing the cells to spread and form new tumors. This unfounded belief may be further influenced by recent research on certain surgical techniques used during hysterectomy procedures, which differ significantly from those used in breast cancer surgery.
Hysterectomy is a widely used and effective treatment for conditions such as uterine fibroids, endometriosis, uterine prolapse and uterine cancer. However, certain surgical techniques—particularly those involving morcellation—carry a low risk of spreading undetected cancer cells within the abdominal or pelvic cavity. In response to this concern, the U.S. Food and Drug Administration (FDA) has issued a safety alert regarding the use of power morcellation in specific cases.
The bottom line is that hysterectomy and breast cancer surgery involve completely different surgical techniques. Furthermore, breast cancer surgery does not cause cancerous cells to become more aggressive or metastasize. If a tumor is found in another part of the body after lumpectomy or mastectomy, it may be because:
- The cancer had already spread before the surgery was performed.
- A new tumor has developed.
- Microscopic cancer cells were left behind during the surgical procedure.
- Cancerous cells entered a blood vessel while the surgeon was removing the tumor.
To help eliminate any remaining microscopic cancer cells after breast cancer surgery, follow-up treatment may be considered, such as radiation therapy, chemotherapy, targeted therapy or hormone therapy. Advances in imaging and pathology are helping physicians detect tumors at earlier stages, reducing the risk of undetected cancer spread.

"My treatment team knew my background and they weren't letting that just go to the side."
Schedule your screening mammogramMisconception #3: Breast-conserving surgery is not an option for a patient with a strong family history of breast cancer.
Breast cancer is not a “one-size-fits-all” diagnosis. There are many different types of breast tumors, which are classified based on their cellular origin. Each type has distinct features and considerations. Therefore, a strong family history of breast cancer does not necessarily mean the tumor is aggressive, nor does it automatically rule out lumpectomy as an option.
To determine the optimal breast cancer treatment approach, the physician and patient will consider multiple individual factors, including the size, location, stage and behavior of the tumor and the patient’s overall health and preferences. Many patients with a family history of breast cancer opt for lumpectomy and achieve an excellent outcome.
Misconception #4: Lymph node removal always results in permanent arm swelling.
Breast cancer surgery often involves removing lymph nodes. For instance, sentinel lymph node mapping and biopsy are used to determine if breast cancer has spread to the lymph nodes in the armpit (axilla). During this procedure, a dye or radioactive tracer is injected near the tumor site. The tracer then travels through the lymphatic system, highlighting the lymph nodes that are most likely to be affected if cancer has spread. The surgeon will remove these sentinel lymph nodes and send them to a lab for microscopic examination by a pathologist, who can identify cancerous cells.
In more advanced cases, axillary lymph node dissection may be performed during breast cancer surgery if lymph node involvement is suspected. This procedure involves removing the lymph nodes from the axilla and analyzing them for the presence of cancer.
Because lymph node removal can disrupt fluid drainage, it may lead to uncomfortable side effects, such as lingering discomfort, numbness and swelling (lymphedema) due to fluid buildup in the affected area of the body, usually the arm. Approximately 20% of patients experience lymphedema after breast cancer surgery with lymph node removal. In general, axillary lymph node dissection carries a higher risk of lymphedema than sentinel lymph node biopsy.
Although lymphedema can develop after breast cancer surgery, it is not a given. Physical therapy, targeted exercises and proper post-surgical care can both minimize the risk and reduce the severity of the condition.
Florida's Cancer Center of Excellence
Moffitt is a Cancer Center of Excellence by the state of Florida. The designation recognizes providers that exceed service standards and excel in providing quality, comprehensive and patient-coordinated care.
Misconception #5: Surgery alone always cures breast cancer.
Surgery has been a mainstay of breast cancer treatment for many decades, but it does not offer a guaranteed cure. Neither lumpectomy nor mastectomy can remove cancer that has already spread beyond the breast to other parts of the body.
To enhance treatment effectiveness, breast cancer surgery is often part of a broader care plan that includes radiation therapy, chemotherapy, hormone therapy or targeted therapy. This multispecialty approach allows for a personalized treatment plan designed to improve the outcome and support the patient’s overall quality of life.
Misconception #6: If a titanium clip is left in a breast after a biopsy, the clip can damage the breast or travel to other parts of the body.
Since the late 1990s, titanium marker clips have been used to identify areas of concern within breast tissue. These small clips are typically placed during an image-guided needle biopsy to mark the location of suspicious cells. Because the clips are visible on X-rays and other imaging scans, they can serve as a reliable guide for a surgeon when evaluating or planning breast cancer surgery.
If surgery is performed, the clip will be removed along with the targeted breast tissue. However, if surgery is deemed unnecessary, the clip can safely remain in place; there is no medical need to remove it unless a rare allergic reaction occurs. The clip will not damage the breast tissue, nor will it migrate to other areas of the body. In some cases, it may be used to monitor a benign breast condition over time.
Benefit from world-class care at Moffitt Cancer Center
Breast cancer surgery is a highly individualized treatment, and ongoing advancements in surgical techniques continue to enhance both clinical outcomes and cosmetic results. At Moffitt, we encourage every patient to explore all available options—including participation in clinical trials—in close collaboration with a trusted care team. Our experienced surgeons work alongside supportive care specialists to provide personalized treatment recommendations tailored to each patient’s unique diagnosis and preferences. We are committed to addressing our patients’ questions and concerns with honesty, clarity and compassion.
Whether you are weighing your surgical treatment options or seeking to separate fact from fiction, we are here to help you make informed decisions with confidence. You can request an appointment with a specialist in Moffitt’s nationally acclaimed Don & Erika Wallace Comprehensive Breast Program by calling 1-888-663-3488 or submitting a new patient registration form online. We do not require referrals.